Menopause is a natural biological process that marks the end of a woman’s reproductive years. It is defined as the point in time when menstrual cycles permanently cease due to the natural depletion of ovarian oocytes from aging. The transition to this stage is often accompanied by a variety of symptoms and changes in the body, largely due to alterations in hormone levels. Menopause is significant not only because it signals the end of fertility but also because it can impact a woman’s health, quality of life, and risk for certain diseases.
Understanding the Typical Age Range for Menopause
The average age for reaching menopause is 51, although it can occur anytime from the 30s to the mid-50s or later. Factors such as genetics, health, and lifestyle can influence the timing of menopause. For instance, women who smoke or are underweight may experience an earlier onset, while those who are overweight might have a later onset. It’s important to note that menopause is considered to be “complete” after a woman has gone without menstruating for one continuous year.
Overview of Early and Premature Menopause
While the average age of menopause is 51, some women go through this transition earlier. Early menopause refers to menopause that occurs before the age of 45. Premature menopause, also known as premature ovarian insufficiency (POI), is when menopause happens before the age of 40. These conditions are relatively rare, with early menopause affecting about 5% of women and premature menopause affecting 1%. The causes can be natural or induced, such as from surgery or medical treatments like chemotherapy. The symptoms of early and premature menopause are similar to those experienced during the typical age range but can have more significant health implications due to the longer duration of life without the protective effects of estrogen.
Distinguishing Between Early and Premature Menopause
Age Criteria for Early and Premature Menopause
Menopause is a natural biological process marking the end of a woman’s reproductive years. However, the timing of this event can vary significantly. Early menopause is characterized by the cessation of menstruation before the age of 45. In contrast, premature menopause refers to menopause occurring before the age of 40. It is important to note that these age criteria are not arbitrary but are based on statistical averages, with the typical age for menopause being around 51 years.
While early menopause affects approximately 5% of women, premature menopause is less common, occurring in about 1% of individuals assigned female at birth (AFAB). The rarest occurrence is menopause before the age of 30, which happens in roughly 0.1% of people AFAB. Recognizing the age at which menopause occurs is crucial for diagnosis and subsequent management of the condition.
Clinical Differences and Terminology
The terms “early” and “premature” menopause are often used interchangeably, but they signify different age-related thresholds. Despite this difference, both conditions can share similar causes and health implications. The cessation of ovarian hormone production and the end of menstrual cycles are common to both, leading to the inability to conceive naturally.
It is also essential to distinguish between premature menopause and premature ovarian insufficiency (POI), formerly known as premature ovarian failure. POI is a condition where menstrual periods stop suddenly and spontaneously at an early age, which may be either early or premature. However, unlike early or premature menopause, individuals with POI may still have intermittent ovarian function, allowing for possible ovulation, menstruation, or even pregnancy. In contrast, once early or premature menopause has occurred, the loss of reproductive capability is permanent.
Understanding these distinctions is vital for healthcare providers and patients alike, as they have different prognoses and treatment approaches. For instance, hormone replacement therapy (HRT) may be recommended for women experiencing early or premature menopause to mitigate long-term health risks, whereas management of POI might focus on addressing fertility concerns and the possibility of intermittent symptoms.
In summary, while early and premature menopause are similar in their cessation of menstrual periods and end of natural fertility, they are differentiated by the age at onset. Additionally, the clinical terminology used to describe these conditions reflects their distinct prognostic and therapeutic considerations.
Premature Ovarian Insufficiency (POI) vs. Menopause
Defining POI and Its Symptoms
Primary Ovarian Insufficiency (POI), previously known as premature ovarian failure, is a condition characterized by the malfunctioning of the ovaries in a woman under the age of 40. Unlike natural menopause, which is the cessation of menstrual periods around the average age of 51, POI can begin as early as the teenage years. Women with POI may experience irregular periods and reduced fertility prematurely. The symptoms of POI often mirror those of menopause and can include:
- Irregular or missed periods
- Hot flashes
- Night sweats
- Irritability and mood swings
- Poor concentration
- Decreased libido
- Pain during intercourse
- Vaginal dryness
For many, the struggle with infertility is the catalyst for seeking medical advice and ultimately receiving a diagnosis of POI.

From unhappy, dry, and sandpaper to silky, smooth and feeling good. That’s Cleo. Cleo is a 100% natural labial balm to moisture and soothe “your other lips”. Cleo is chemical-free, water-free, pH optimized and helps maintain and restore your delicate labial skin’s natural flora. Ideal for daily use or as needed. Get the most silky, lovable lips ever.
Comparing POI with Early and Premature Menopause
While POI and early or premature menopause share similar symptoms, they are distinct conditions. Early menopause refers to the cessation of menstrual periods between the ages of 40 and 45, whereas premature menopause occurs before age 40. In both cases, ovulation ceases, menstruation ends, and pregnancy becomes impossible without medical intervention. Conversely, POI is characterized by intermittent and unpredictable ovarian function. This means that some women with POI may still ovulate occasionally, have menstrual cycles, and even conceive, despite the reduced fertility.
Fertility Implications of POI
The fertility implications of POI are significant, as the condition often leads to difficulties in conceiving. While not synonymous with absolute infertility, the sporadic ovulation associated with POI reduces the chances of natural conception. Women with POI who wish to become pregnant may need to explore assisted reproductive technologies such as in vitro fertilization (IVF). It is important to note that even with IVF, donor eggs may be necessary due to the compromised quality of the patient’s own eggs. The emotional and psychological impact of these fertility challenges can be profound, necessitating a compassionate and comprehensive approach to treatment and support.
Causes of Early and Premature Menopause
Genetic Factors and Family History
Genetic predispositions play a significant role in determining the onset of menopause. A family history of early or premature menopause can be a strong indicator that a similar pattern may follow in offspring. Specific genetic disorders, such as Turner’s syndrome (45X0) and Fragile X syndrome, are associated with premature ovarian failure, leading to early menopause. Genetic counseling may provide insights into the risk and management of early menopause for those with a family history or known genetic conditions.
Autoimmune Disorders and Other Medical Conditions
Autoimmune disorders are among the leading causes of premature ovarian insufficiency (POI), which can lead to early menopause. Conditions such as thyroiditis, rheumatoid arthritis, and systemic lupus erythematosus can cause the immune system to mistakenly attack ovarian tissue, reducing estrogen production and leading to menopause symptoms. Other medical conditions, including epilepsy and certain metabolic syndromes, have also been linked to early menopause.
Lifestyle and Environmental Factors
Lifestyle choices and environmental exposures can influence the timing of menopause. Smoking has a dose-related effect on the age of menopause onset, with smokers likely to experience menopause earlier than non-smokers. Other factors such as poor nutrition, excessive alcohol consumption, and exposure to toxins can also contribute to the early decline of ovarian function.
Surgical and Medical Interventions
Medical treatments and surgeries can induce early menopause. For instance, a bilateral oophorectomy, the surgical removal of both ovaries, results in immediate menopause, regardless of the patient’s age. Chemotherapy and pelvic radiation therapy for cancer treatment can damage the ovaries, leading to temporary or permanent menopause. The risk of ovarian failure increases with the dosage and type of chemotherapy, as well as the patient’s age at the time of treatment.
In conclusion, early and premature menopause can result from a complex interplay of genetic, autoimmune, lifestyle, and medical factors. Understanding these causes is crucial for early detection, management, and support for those experiencing early menopause.
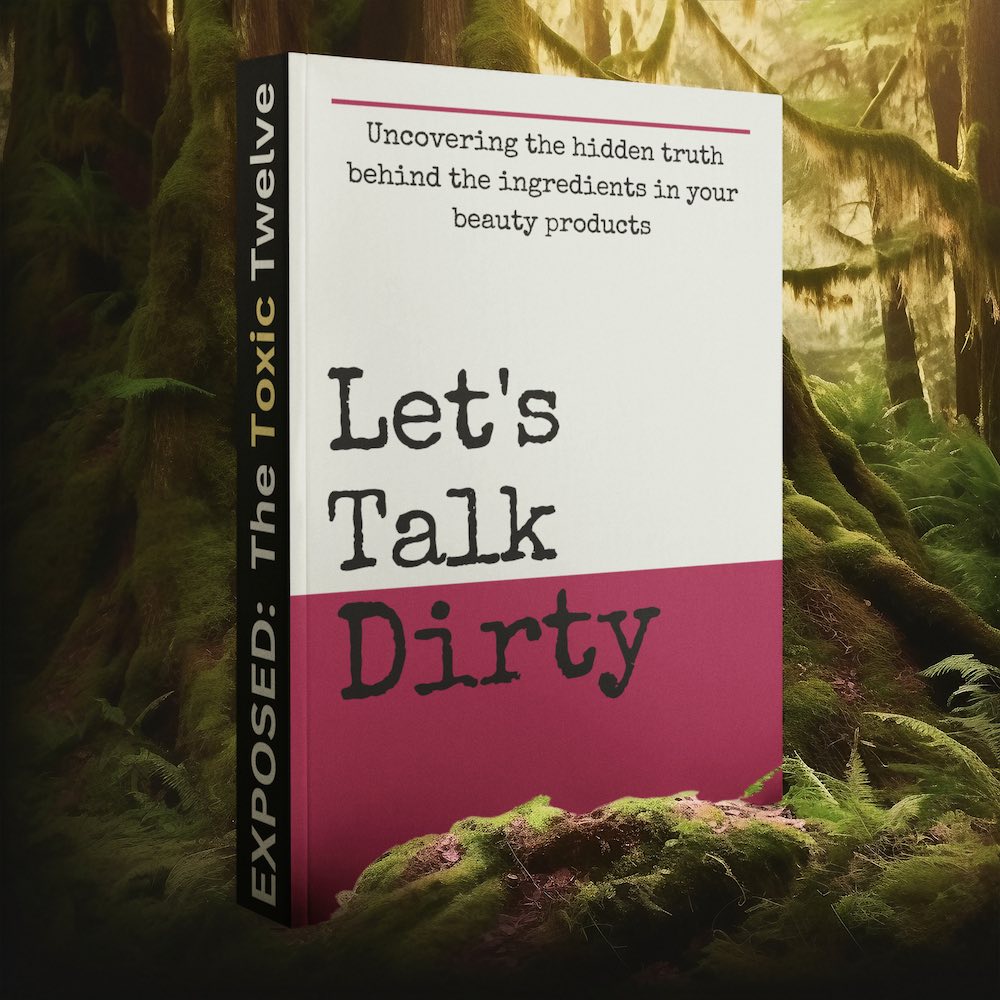
Feeling You Have a Right to Safe Beauty & Fem Care?
If so, it may be time for a change. It starts with knowledge. We have a few suggestions in our new guides.
Symptoms and Health Implications
Common Symptoms of Early and Premature Menopause
Women experiencing early or premature menopause often deal with symptoms similar to those of natural menopause, though they may occur at a more intense level. Common symptoms include:
- Irregular or missed periods: This is often one of the first signs, with periods that may be heavier or lighter than usual.
- Vasomotor symptoms: Hot flashes and night sweats are prevalent, indicating fluctuating estrogen levels.
- Vaginal dryness: Decreased estrogen can lead to discomfort and dryness, often resulting in painful intercourse (dyspareunia).
- Urinary issues: Increased frequency, urgency, and incontinence may occur due to changes in the urinary tract.
- Emotional changes: Mood swings, irritability, and increased risk of depression can affect mental health.
- Sexual dysfunction: A decrease in libido and discomfort during sex due to vaginal dryness.
- Sleep disturbances: Insomnia and sleep disruptions are common, sometimes exacerbated by night sweats.

Long-Term Health Risks Associated with Early Menopause
Early menopause extends the period of estrogen deficiency, increasing the risk of several long-term health issues:
- Osteoporosis: The prolonged lack of estrogen accelerates bone density loss, heightening the risk of fractures and osteoporosis.
- Cardiovascular disease: Estrogen has a protective effect on heart health; its early loss can lead to an increased risk of heart disease and stroke.
- Neurological diseases: Some studies suggest a link between early menopause and an increased risk of neurological conditions.
- Premature death: The overall risk of premature mortality may be elevated due to the associated health risks.
Psychological and Emotional Impact
The psychological and emotional impact of early and premature menopause can be profound. Women may experience:
- Grief and loss: Feelings of loss related to fertility and the end of menstrual cycles can be significant.
- Body image concerns: Changes in physical appearance and sexual function can affect self-esteem and body image.
- Fertility concerns: The inability to conceive naturally can be distressing for those who desire to have children.
- Sexuality and intimacy: Changes in sexual function and desire can strain intimate relationships.
- Mental health: Increased risks of depression, anxiety, and mood disorders are associated with the hormonal changes of menopause.
It is crucial for women undergoing early or premature menopause to seek support, whether through counseling, support groups, or medical advice, to manage these psychological and emotional challenges effectively.
Diagnosis and Monitoring
Medical Tests and Diagnosis Criteria
Diagnosing premature and early menopause requires a careful review of symptoms, medical history, and specific blood tests. The most common tests include:
- Follicle-stimulating hormone (FSH): Elevated levels of FSH, typically above 30 milli-international units per milliliter (mIU/mL), can indicate reduced ovarian function. However, because hormone levels fluctuate, a single elevated FSH test is not definitive.
- Estrogen (Estradiol): Low levels of estrogen are consistent with menopause.
- Anti-Müllerian hormone (AMH): AMH levels can help assess the remaining egg supply, or ovarian reserve, which decreases as menopause approaches.
- Thyroid-stimulating hormone (TSH): Since thyroid disorders can mimic menopausal symptoms, TSH levels are checked to rule out thyroid issues.
It’s important to note that while these tests can be helpful, they are not always necessary for diagnosis. Many women are able to recognize the transition based on symptoms alone. However, for those under 40, confirming the diagnosis through testing is crucial to rule out other conditions and to begin appropriate management.
Monitoring and Managing Symptoms
Once diagnosed with premature or early menopause, regular follow-up appointments are essential for monitoring health risks and managing symptoms. Women may be referred to specialists such as endocrinologists, gynecologists, and mental health professionals. Monitoring includes:
- Cardiovascular health: Regular checks of blood pressure, cholesterol, and glucose levels, as women with premature or early menopause are at increased risk for cardiovascular disease.
- Bone density: Assessments for osteoporosis, since early menopause can lead to a more rapid loss of bone density.
- Vasomotor symptoms: Management of hot flashes, night sweats, and other symptoms through lifestyle changes or hormone replacement therapy (HRT).
- Vaginal and sexual health: Addressing issues like vaginal dryness or decreased libido, which can affect quality of life and intimate relationships.
- Mental health: Evaluating for depression, anxiety, and mood changes, as these can be more prevalent in women experiencing premature or early menopause.
For symptom relief, doctors may prescribe hormone therapy until the average age of natural menopause, typically around 51. Hormone therapy can mitigate long-term health risks such as osteoporosis and cardiovascular disease. However, it’s not without side effects and risks, which should be discussed with a healthcare provider.
Emotional well-being is also a critical aspect of managing premature and early menopause. Support from healthcare providers, counseling, and open communication with partners and family can help women navigate the psychological and emotional challenges associated with this condition.
Treatment and Management Strategies
Hormone Replacement Therapy (HRT) and Alternatives
Hormone Replacement Therapy (HRT) is a widely used treatment for managing the symptoms of early and premature menopause. HRT involves the administration of estrogen and, in women with a uterus, progesterone to mitigate the effects of hormonal deficiencies. This therapy can alleviate vasomotor symptoms, such as hot flashes and night sweats, and help prevent long-term consequences like osteoporosis. However, HRT is not suitable for everyone. It is crucial to discuss the potential risks and benefits with a healthcare provider.
For those who cannot or choose not to use HRT, alternatives include non-hormonal medications like selective serotonin reuptake inhibitors (SSRIs) or gabapentin, which can reduce hot flashes. Phytoestrogens, which are plant-derived compounds with estrogen-like properties, and lifestyle changes may also provide relief for some symptoms.
Lifestyle Modifications and Support Systems
Adopting a healthy lifestyle can play a significant role in managing menopause symptoms. Regular physical activity can improve mood, weight management, and bone health. A balanced diet rich in calcium and vitamin D is essential for bone strength. Avoiding triggers for hot flashes, such as spicy foods, caffeine, and alcohol, can also be beneficial. Additionally, support systems, including counseling, support groups, and educational resources, can provide emotional support and help women navigate the challenges of early and premature menopause.
By the way, something for you, a little gift!!!
I am just in the middle of publishing my book. It’s about How women can balance their hormones. One part is about food and diet, of course.
Follow this link and enter your email.
I will send you this part of the book for free once the book is published. It has many concrete, practical tips and recipes and will help you feel better during menopause or times of Big hormonal fluctuations.
Annette, Damiva Lead for Health & Wellness

Fertility Options and Family Planning
For women who experience early or premature menopause but wish to have children, there are several fertility options. These include assisted reproductive technologies such as in vitro fertilization (IVF) with donor eggs. Adoption is another pathway to parenthood that can be considered. It is important to consult with a fertility specialist to understand the available options and the likelihood of success based on individual circumstances.
Mental Health Support and Counseling
The psychological and emotional impact of early and premature menopause can be significant. Women may experience feelings of loss, anxiety, and depression. Seeking mental health support through therapy or counseling can be an effective way to address these challenges. Cognitive-behavioral therapy (CBT) has been shown to help with mood swings and depression. Mindfulness and stress reduction techniques can also be beneficial in managing the emotional aspects of menopause.
In conclusion, the treatment and management of early and premature menopause require a multifaceted approach that includes medical interventions, lifestyle changes, and emotional support. It is essential for women to work closely with their healthcare providers to develop a personalized plan that addresses their specific needs and concerns.