Welcome, this is cervical polyps video part three of four. I’ll dive deeply into why we get polyps.
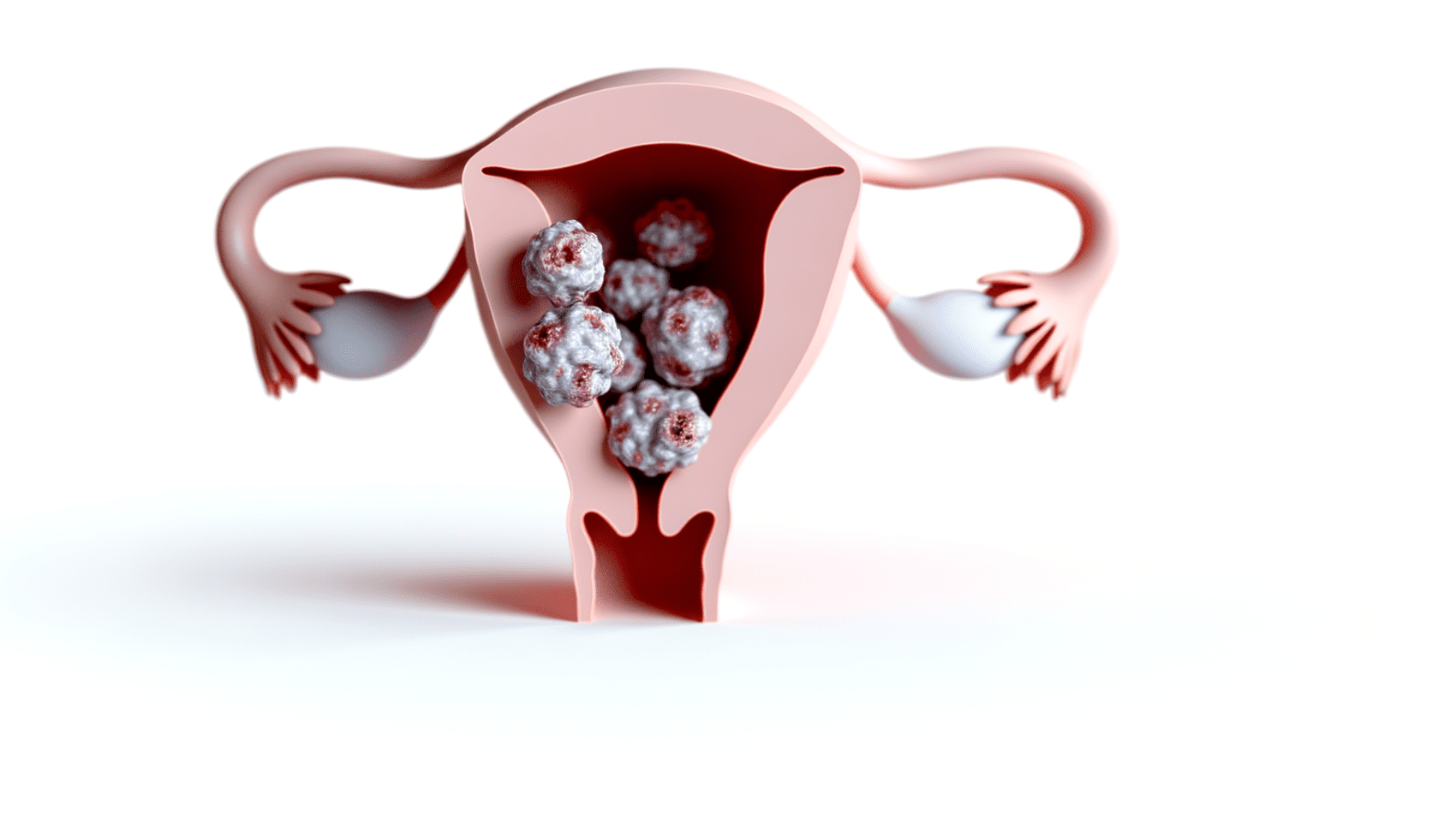
As I mentioned in video one, cervical polyps are small, irregular growths on the surface of your cervix or in your cervical canal.
Your cervix connects your uterus to your vagina.
So why do we get them?
I mentioned earlier that cervical polyps may be caused by chronic inflammation, which may involve infections, medical conditions, or environmental factors.
Let me go over the list now. Here are the common causes.
First, chronic infections. These are persistent or reoccurring infections and are a leading cause of chronic inflammation and they can include sexually transmitted infections or STIs such as HPV, the human papillomavirus, chlamydia, gonorrhea, and herpes simplex virus.
And just as a note, HPV can also result in cervical cancer.
Bacterial vaginosis. This condition is characterized by an imbalance in the normal bacteria in the vagina.
Yeast infections caused by an overgrowth of Candida albicans or other Candida species in the vagina.
Number two, chemical irritants.
Exposure to chemical irritants can cause chronic inflammation. This might include douches and vaginal sprays that disrupt the normal vaginal flora. Latex in condoms or diaphragms. Thanks for watching! Spermicide used for birth control.
Number three, the presence of foreign bodies.
For example, a forgotten tampon. And this, for instance, can lead to inflammation and infection.
Number four, hormonal imbalances.
Fluctuations in hormone levels, especially estrogen and progesterone. This can affect the vaginal environment and contribute to inflammation.
Number five, autoimmune disorders. Conditions where the body’s immune system attacks its own tissue can lead to inflammation in various parts of the body, including the reproductive tract.
Number six, chronic medical conditions.
Conditions such as diabetes, which can affect the immune system, may increase the risk of infections and subsequent inflammation.
Number seven, mechanical irritation.
Physical irritants such as frequent sexual intercourse or certain gynecological procedures can cause mechanical irritation leading to inflammation.
Number eight, tamoxifen.
Women treated with tamoxifen for breast cancer may experience changes in the vaginal and uterine environment, leading to inflammation.
Let’s take a deeper look at number four, the hormonal imbalances.
Fluctuations in hormone levels, particularly estrogen and progesterone, can indeed affect the vaginal environment and contribute to inflammation.
These hormonal changes can also influence the development of polyps in the reproductive system, including both cervical and, endometrial or uterine polyps.
And here’s how. So first, hormonal influence on tissue growth.
We know that estrogen plays a key role in stimulating the growth of endometrial lining of the uterus and also affects the cervix and vaginal tissues. When estrogen levels are high, it can lead to excessive growth of these tissues.
Progesterone typically counterbalances estrogen’s effects by regulating the growth and shedding of the endometrial lining.
Imbalances in these hormones, particularly when estrogen is high relative to progesterone, can lead to abnormal tissue growth, such as polyps.
Second, inflammation and polyp formation.
Chronic inflammation which can be exacerbated by hormonal imbalances can contribute to an environment which is conducive to the development of polyps.
Inflammation is a process involving your body’s immune response that can lead to tissue damage and repair. During the repair process, the affected tissue may undergo changes that predispose them to abnormal growths, including polyps.
Number three, vascular effects.
Hormones, especially estrogen, have effects on blood vessels, promoting blood flow to the reproductive organs. Increased blood flow and vascular changes associated with hormonal fluctuations can support the growth of polyps by providing them with an Increased supply of nutrients and oxygen.
Number four, cell proliferation.
Estrogen promotes cell proliferation, which is the process by which cells divide and multiply, and this can lead to the overgrowth of cells in the lining of the uterus, in the endometrium, or the cervix, contributing to the formation of polyps.
Number five, reproductive system sensitivity.
The tissue of the reproductive system, including the endometrium and cervix, are particularly sensitive to estrogen and progesterone. This sensitivity means that any imbalance in these hormones can have a pronounced effect on tissue behavior, including the potential for polyp development.
In summary, while hormonal fluctuations can affect the vaginal environment and contribute to inflammation, these hormonal changes, particularly those involving estrogen and progesterone, play a significant role in the development of polyps by promoting tissue growth affecting blood vessels and causing changes in the reproductive systems tissues.
So it’s super important to balance your hormones and this when hormones are changing in reproductive years fluctuating erratically in perimenopause and when declining in the postmenopausal years.
So I hope you found this video informative. Be sure to join me in part four where I’ll show you what you can do to positively affect your health, balance your hormones, and decrease inflammation in your body.