Understanding Melasma: Definition and Symptoms
Melasma is a common skin condition characterized by the development of brown to gray-brown patches, primarily on the face. These patches often appear on the cheeks, chin, nose bridge, forehead, and above the upper lip. While melasma can affect anyone, it is more prevalent in women than men, particularly during reproductive years. The condition is also linked to hormonal changes, such as those occurring during pregnancy, and the use of oral contraceptives and hormone therapies.
The Link Between Melasma and Menopause
Menopause, a natural biological process marking the end of a woman’s menstrual cycles, can be a significant period for the onset or exacerbation of melasma. The hormonal fluctuations associated with menopause, especially changes in estrogen and progesterone levels, may contribute to the development of melasma. This connection underscores the importance of understanding hormonal influences on skin pigmentation.
Psychological Impact of Melasma
The appearance of melasma can have a profound psychological impact on individuals, affecting self-esteem and quality of life. The visibility of the condition, particularly on the face, can lead to social anxiety and emotional distress. It is essential to acknowledge the psychological aspect of melasma and provide support to those affected.
Scope of the Article
This article aims to explore the multifaceted relationship between melasma and menopause, delving into the epidemiology, pathophysiology, and treatment options available. By examining the hormonal changes during menopause that may influence melasma, we can better understand the condition and improve the management strategies for those experiencing it.
Epidemiology and Demographics
Prevalence Among Different Populations
Melasma is a chronic acquired hypermelanosis that presents as irregular brown macules, predominantly on sun-exposed areas of the body. Its prevalence varies significantly across different populations, influenced by factors such as ethnic composition, skin phototype, and sun exposure. While melasma can affect individuals of any ethnic background, it is more prevalent among those with more pigmented phenotypes, such as East Asians, Indians, Middle Easterners, and Mediterranean-Africans. In the United States, it is commonly seen among Hispanic-Americans, and in Brazil, it affects a significant portion of women living in intertropical regions with high ultraviolet radiation exposure.
Gender Disparities in Melasma Occurrence
Melasma exhibits a clear gender disparity, affecting women far more frequently than men. The female to male ratio of melasma occurrence can range from 9:1 to as high as 39:1 in certain populations. This disparity is attributed to hormonal influences, particularly the roles of estrogen and progesterone, which are known to stimulate melanocytes and increase melanin production when the skin is exposed to sunlight.
Age and Hormonal Factors
The onset of melasma is most common during the reproductive years, with a majority of cases developing between the ages of 20 and 40. Hormonal factors play a significant role in the pathophysiology of melasma, with pregnancy, use of oral contraceptives, and hormone replacement therapy being common triggers. The condition is often referred to as the “mask of pregnancy” due to its frequent occurrence during this time. The hormonal relationship is further supported by the observation that melasma is more persistent in women who have used oral contraceptives and tends to recur with subsequent pregnancies.
Overall, the epidemiology of melasma underscores the importance of understanding the interplay between genetic predisposition, hormonal factors, and environmental triggers in managing this condition effectively.
Do you have the most commonly used but toxic, disease bringing chemicals in your skin care? Many chemicals in skincare are hormone disruptors and make menopause symptoms worse.
Find out more…
Pathophysiology of Melasma
Role of Melanocytes and Melanin
Melasma is characterized by the overproduction of melanin, the pigment responsible for skin color, which leads to the appearance of brown to gray-brown patches on the face. Melanocytes, the cells that produce melanin, are stimulated to increase melanin synthesis by various factors, including hormonal changes, genetic predisposition, and environmental triggers. The distribution of melanin across the epidermis is not uniform in melasma, with a higher concentration in the basal and suprabasal layers. This uneven melanin distribution contributes to the patchy appearance of the condition.
Hormonal Influences on Skin Pigmentation
Hormones, particularly estrogen and progesterone, are known to influence melanocyte activity. During menopause, fluctuations in hormone levels can exacerbate melasma. Estrogen and progesterone receptors are found on melanocytes, and their activation leads to increased melanin production. Hormone Replacement Therapy (HRT), commonly used during menopause, can impact melanocyte activity and potentially trigger or worsen melasma in susceptible individuals.
Genetic Factors and Melasma
Genetic predisposition plays a significant role in the development of melasma. Studies have shown that individuals with a family history of melasma are more likely to develop the condition themselves. Genetic factors may influence the responsiveness of melanocytes to hormonal and environmental stimuli, making certain populations more prone to melasma.
Environmental Triggers
Exposure to ultraviolet (UV) radiation from the sun is a major environmental trigger for melasma. UV radiation can induce the production of melanocyte-stimulating hormone (MSH), leading to increased melanin synthesis. Additionally, visible light and infrared radiation have also been implicated in the pathogenesis of melasma. Protective measures, such as the use of broad-spectrum sunscreens, are crucial in managing melasma, particularly during menopause when skin may become more sensitive to environmental factors.
In conclusion, the pathophysiology of melasma is multifactorial, involving a complex interplay between melanocytes, hormones, genetic predisposition, and environmental factors. Understanding these underlying mechanisms is essential for the development of targeted treatments and preventive strategies for managing melasma during menopause.
Melasma and Hormonal Changes During Menopause
Estrogen, Progesterone, and Melanocyte Activity
During menopause, the hormonal landscape of a woman’s body undergoes significant changes, particularly in the levels of estrogen and progesterone. These hormones are known to influence the activity of melanocytes, the cells responsible for producing melanin, the pigment that gives skin its color. Elevated levels of estrogen and progesterone can stimulate melanocytes to produce more melanin, leading to the development of melasma, a condition characterized by dark, discolored patches on the skin. This is particularly evident during menopause when hormonal fluctuations are at their peak.
Impact of Hormone Replacement Therapy
Hormone Replacement Therapy (HRT) is commonly used to alleviate menopausal symptoms by supplementing estrogen and progesterone levels. However, HRT can have a dual effect on melasma. While it can relieve certain menopausal symptoms, it may also exacerbate melasma in some women by increasing hormone levels that stimulate melanocyte activity. It is crucial for women undergoing HRT to monitor their skin closely and consult with a dermatologist if they notice any changes in pigmentation.
Stress, Cortisol, and Melasma
Menopause can be a stressful time for many women, and stress has been shown to play a role in the exacerbation of melasma. The body’s response to stress involves the release of cortisol, a hormone that can lead to an imbalance in estrogen levels. Elevated estrogen can, in turn, upregulate melanocyte-stimulating hormone (MSH) levels, resulting in increased melanin production and the potential worsening of melasma. Managing stress through lifestyle changes, relaxation techniques, and seeking support can be beneficial in controlling the impact of cortisol on skin pigmentation.
Thus, the interplay between hormones and skin health is complex, especially during the transitional phase of menopause. Understanding these relationships is key to managing conditions like melasma. Women experiencing changes in skin pigmentation should seek personalized advice from healthcare providers to navigate these challenges effectively.
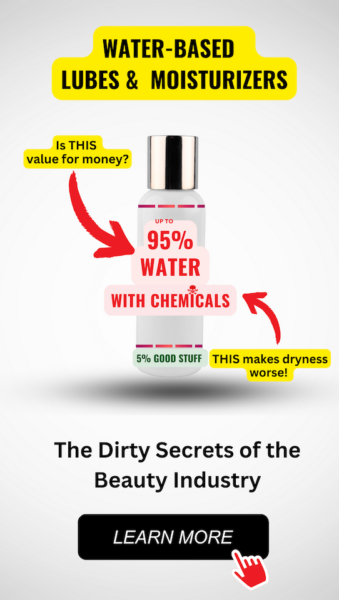
Feeling You Have a Right to Safe Beauty & Fem Care?
If so, it may be time for a change. It starts with knowledge. We have a few suggestions in our new guides.
Natural Management Strategies for Melasma
Sun Protection and Lifestyle Modifications
Melasma, often exacerbated by sun exposure, necessitates rigorous sun protection as a cornerstone of management. Daily application of broad-spectrum sunscreen with a high SPF is essential, and reapplication every two hours is recommended, especially during peak sunlight hours. Physical barriers such as wide-brimmed hats and UV-protective clothing can provide additional defense against UV rays. Lifestyle modifications, including seeking shade and avoiding the sun during its strongest hours, typically between 10 a.m. and 4 p.m., can also reduce the risk of melasma exacerbation.
Dietary Approaches and Anti-Inflammatory Foods
An anti-inflammatory diet rich in antioxidants may help manage melasma from within. Foods high in vitamin C, such as citrus fruits, berries, and leafy greens, can inhibit melanin production and offer photoprotection. Omega-3 fatty acids found in fish like salmon and flaxseeds are known for their anti-inflammatory properties and can support skin health. Additionally, a balanced diet with adequate hydration is fundamental for maintaining overall skin health and may contribute to the management of melasma.
Beneficial Supplements for Skin Health
Certain supplements may complement dietary efforts in managing melasma. Oral supplements containing Polypodium leucotomos, an antioxidant-rich fern extract, have shown promise in treating melasma. Similarly, glutathione, an antioxidant that can lighten pigmentation, may be beneficial when taken orally. However, it is crucial to consult with a healthcare provider before starting any new supplement regimen to ensure safety and appropriateness for individual health needs.
Natural Topical Treatments and Their Efficacy
Natural topical treatments for melasma include ingredients like aloe vera, which has been shown to improve hyperpigmentation in some studies. Topical application of niacinamide (vitamin B3) can also be effective, as it may reduce the transfer of pigment within the skin. Other natural agents such as licorice extract and kojic acid have depigmenting properties and may be found in over-the-counter creams and serums. While these natural treatments can be part of a melasma management plan, their efficacy can vary, and they may work best in conjunction with other treatments. It is important to note that natural does not always mean risk-free, and some natural products can still cause skin irritation or allergic reactions, particularly in sensitive individuals
Medical Interventions and When to Seek Help
Overview of Medical Treatments
When natural management strategies for melasma do not yield the desired results, medical interventions may be considered. The most common medical treatments for melasma include topical agents, chemical peels, and laser therapy. Topical treatments often involve the use of hydroquinone, which inhibits melanin production, and is frequently combined with tretinoin and a corticosteroid in a formulation known as the triple combination or Kligman’s formula. This formula is typically prescribed for a limited duration of three to four months and has shown effectiveness in a significant percentage of patients. Other topical agents include azelaic acid, which can serve as a maintenance treatment post-hydroquinone therapy, and cysteamine, which reduces melanin production and acts as an antioxidant.
In-clinic procedures such as chemical peels and laser therapy are additional options. Chemical peels, using substances like glycolic acid or salicylic acid, can help remove hyperpigmented skin cells. Laser treatments must be approached with caution, as they can lead to complications such as hypo- or hyperpigmentation, especially in individuals with darker skin tones. It is crucial that these treatments are performed under the guidance of a qualified healthcare professional.
Potential Side Effects and Considerations
While medical treatments can be effective, they are not without potential side effects. Hydroquinone, for instance, may cause skin irritation or dermatitis, and in rare cases, may lead to a condition called exogenous ochronosis, which results in blue-black pigmentation. Tretinoin can also cause skin irritation and is not recommended during pregnancy. Chemical peels and laser treatments carry risks such as scarring, infection, and unwanted changes in skin coloration. It is important for patients to be fully informed about the potential risks and to weigh them against the benefits of treatment.
Guidelines for Consulting Healthcare Providers
Consulting with a healthcare provider is essential when considering medical interventions for melasma. Dermatologists are specialists in skin conditions and can provide a comprehensive assessment to determine the most appropriate treatment plan. Patients should seek a dermatologist’s advice if:
- The melasma is causing significant psychological distress or social discomfort.
- Over-the-counter treatments and lifestyle changes have not improved the condition.
- There is a desire to explore prescription medications or professional procedures.
During the consultation, the dermatologist will evaluate the melasma’s characteristics, discuss potential triggers, and review the patient’s medical history, including any medications that may be contributing to the condition. The healthcare provider will also outline the treatment options, expected outcomes, and possible side effects, helping the patient to make an informed decision.
In conclusion, while melasma can be a challenging condition to treat, a range of medical interventions are available. Patients should work closely with their healthcare providers to choose the most suitable treatment and to manage the condition effectively.

Conclusion: Living with Melasma During Menopause
Summarizing Key Points
Menopause is a significant transition in a woman’s life, often accompanied by various physiological changes, including those affecting the skin. Melasma, a common hyperpigmentation disorder, is characterized by brown or gray-brown patches on the face, particularly on the cheeks, bridge of the nose, forehead, and chin. While the exact cause of melasma is not fully understood, it is known to be influenced by hormonal fluctuations, genetic predisposition, and environmental factors such as UV exposure. The psychological impact of melasma on women during menopause can be profound, affecting self-esteem and quality of life.
Emphasizing the Importance of Personalized Care
Effective management of melasma requires a personalized approach that considers the unique circumstances of each individual. Treatment strategies may include a combination of sun protection, topical agents, and procedural interventions. It is crucial for healthcare providers to offer comprehensive care that addresses both the physical and emotional aspects of living with melasma. Education on sun safety, skin care, and the potential benefits and risks of treatments like hormone replacement therapy (HRT) is essential for empowering women to make informed decisions about their health.
Future Directions in Research and Treatment
Despite advancements in understanding melasma, there remains a need for further research to elucidate the pathophysiological mechanisms underlying this condition, particularly in relation to hormonal changes during menopause. Future studies should focus on the development of targeted therapies that can provide more effective and long-lasting results. Additionally, exploring the psychological impact of melasma and integrating psychosocial support into treatment plans will be important for improving overall patient outcomes. As we continue to learn more about melasma and its relationship with menopause, the goal is to enhance the quality of life for women experiencing this skin condition.