Uterine Prolapse
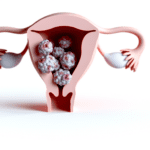
Uterine prolapse is a condition characterized by the descent of the uterus into or beyond the vaginal canal due to weakened support structures. This pelvic floor disorder can range from mild, where the uterus sags into the upper vagina, to severe, where the uterus protrudes completely outside the vaginal opening. The stages of uterine prolapse are classified from Stage I, indicating a minor descent, to Stage IV, which is a complete prolapse.
Prevalence and Demographics
Uterine prolapse is a relatively common condition, particularly among women between the ages of 50 and 79. The likelihood of experiencing uterine prolapse increases with age and is influenced by factors such as childbirth, menopause, and obesity. Globally, the prevalence varies, with some regions like Nepal reporting rates as high as 7% among their female population. It is important to note that while uterine prolapse can significantly impact quality of life, it is not life-threatening.
Importance of Awareness and Treatment
Recognizing the symptoms of uterine prolapse is crucial for timely intervention and management. Symptoms can include a sensation of heaviness or bulging in the vagina, urinary incontinence, and discomfort during physical activities. Awareness and understanding of uterine prolapse can lead to early diagnosis and treatment, which may include pelvic floor exercises, pessary insertion, or surgery. Treatment not only improves physical symptoms but also addresses psychological and social implications, enhancing overall quality of life. Healthcare providers play a vital role in educating patients about the condition, its potential complications, and the importance of seeking medical attention when symptoms arise.
Anatomy and Physiology
Normal Position and Function of the Uterus
The uterus is a dynamic organ central to the female reproductive system, primarily responsible for menstruation, pregnancy, and labor. Anatomically, it is positioned in the pelvis, posterior to the bladder and anterior to the rectum. The uterus is held in place by several structures, including the pelvic floor muscles, ligaments, and connective tissues. These supportive elements allow the uterus to maintain its position while accommodating the changes that occur during the menstrual cycle and pregnancy.
Supportive Pelvic Structures
The pelvic floor muscles, a complex network of muscles stretching like a hammock from the pubic bone to the tailbone, play a crucial role in supporting the uterus and other pelvic organs. Ligaments such as the uterosacral and cardinal ligaments also provide support by connecting the uterus to the sacrum and the lateral pelvic walls. Additionally, the round ligaments help to keep the uterus in an anteverted position. These structures work in concert to maintain the normal anatomical position of the uterus and accommodate the increased weight during pregnancy.
Impact of Prolapse on Pelvic Anatomy
Uterine prolapse occurs when the muscles, ligaments, and connective tissues that support the uterus become weakened or damaged. This can lead to the descent of the uterus into the vaginal canal, which may progress to the point where the uterus protrudes outside the vagina in severe cases. The stages of uterine prolapse are classified based on the degree of descent. The impact of prolapse on pelvic anatomy can be profound, often leading to a domino effect where the weakening of one pelvic structure can cause subsequent prolapse of adjacent organs, such as the bladder (cystocele) or rectum (rectocele).
The displacement of the uterus can significantly alter the normal function of the pelvic organs, potentially causing urinary and bowel incontinence, sexual dysfunction, and a host of other physical discomforts. The psychological and social implications of these changes can also be significant, affecting a woman’s quality of life and self-esteem. Therefore, understanding the anatomy and physiology of the pelvic region is essential for recognizing the early signs of prolapse and seeking timely medical intervention.
Symptoms of Uterine Prolapse
Early Stage Symptoms
In the initial stages of uterine prolapse, many women may not experience any noticeable symptoms. However, as the condition progresses, some may begin to feel a sense of heaviness or fullness in the pelvic area. This can be accompanied by a slight bulge in the vagina that is not always visible but may be felt as a protrusion or lump. Other early stage symptoms can include:
- A sensation of sitting on a small ball
- Discomfort or pain during sexual intercourse
- Minor lower back pain
- Difficulty with inserting tampons or vaginal applicators
Moderate to Severe Prolapse Symptoms
As uterine prolapse advances to moderate or severe stages, symptoms typically become more pronounced. Women may notice:
- Visible tissue protruding from the vagina, which may appear as a bulge or, in severe cases, like a red ball coming out of the vaginal opening.
- Increased discomfort or pain in the pelvic region, lower back, or during intercourse.
- Urinary problems, such as leakage of urine (incontinence), a frequent urge to urinate, or difficulty emptying the bladder completely.
- Bowel movement issues, including constipation or the need to press on the vaginal wall to complete a bowel movement.
Symptoms Indicative of Complications
Some symptoms may suggest the development of complications due to uterine prolapse and require immediate medical attention:
- Urinary retention or an inability to pass urine, which can lead to kidney damage.
- Severe bulging of the uterus outside the vagina, potentially leading to ulceration or infection.
- Complete uterine prolapse, where the uterus is entirely outside of the vaginal opening.
Psychological and Social Implications
The symptoms of uterine prolapse can extend beyond physical discomfort, potentially leading to psychological and social implications. Women may experience:
- Anxiety and depression due to chronic discomfort or pain and concerns about body image.
- Sexual dysfunction, which can arise from pain during intercourse or embarrassment about the condition.
- Social withdrawal or reduced quality of life as a result of the symptoms interfering with daily activities and personal relationships.
It is important for women experiencing any of these symptoms to seek medical advice, as early detection and treatment can significantly improve quality of life and prevent progression to more severe stages.

Causes and Risk Factors
Biological and Physical Causes
The primary biological and physical causes of uterine prolapse are related to the weakening of the muscles, ligaments, and connective tissues that support the uterus. This weakening can occur due to a variety of factors:
- Vaginal Childbirth: Multiple or difficult vaginal deliveries can stretch and weaken pelvic floor muscles.
- Menopause: The decrease in estrogen levels during menopause can lead to a reduction in the strength and resilience of pelvic tissues.
- Age: Natural aging processes can cause muscles to lose tone and strength.
- Chronic Constipation: Repeated straining during bowel movements can stress pelvic muscles.
- Chronic Cough: Persistent coughing increases pressure on pelvic organs and can weaken support structures.
- Heavy Lifting: Regularly lifting heavy objects can strain pelvic floor muscles.
Lifestyle and Environmental Factors
Lifestyle choices and environmental factors can also contribute to the development of uterine prolapse:
- Obesity: Carrying excess weight increases the strain on pelvic structures.
- Physical Activity: Lack of regular exercise can lead to weaker pelvic muscles.
- Diet: A diet low in fiber can lead to constipation and subsequent straining.
- Smoking: Smoking can lead to chronic coughing and reduced blood flow to pelvic tissues, both of which can contribute to prolapse.
Genetic Predispositions and Family History
Genetics may play a role in the likelihood of developing uterine prolapse. A family history of uterine prolapse or pelvic organ prolapse can indicate a genetic predisposition to weaker connective tissue in the pelvic area. Additionally, certain ethnic backgrounds, such as White or Hispanic descent, have been associated with a higher risk of prolapse.
In conclusion, uterine prolapse is a multifactorial condition influenced by a combination of biological, lifestyle, and genetic factors. Understanding these risk factors can help in the prevention and management of uterine prolapse, and it is important for individuals to discuss their risk with healthcare providers, especially if they have a family history or are experiencing symptoms indicative of prolapse.
By the way, something for you, a little gift!!!
I am just in the middle of publishing my book. It’s about How women can balance their hormones. One part is about food and diet, of course.
Follow this link and enter your email.
I will send you this part of the book for free once the book is published. It has many concrete, practical tips and recipes and will help you feel better during menopause or times of Big hormonal fluctuations.
Annette, Damiva Lead for Health & Wellness

Diagnosis and When to Seek Medical Attention
Diagnostic Procedures
Diagnosing uterine prolapse typically begins with a thorough medical history and a physical examination of the pelvis. During the exam, healthcare providers assess the position of the uterus and the strength of the pelvic floor muscles. A cystoscopy may be performed if urinary incontinence or incomplete bladder emptying is a concern, allowing the doctor to examine the bladder and urethra. Additionally, an MRI (magnetic resonance imaging) might be ordered to provide detailed images of the kidneys and other pelvic organs, helping to rule out other conditions and to determine the extent of the prolapse.
Interpreting Symptoms and Self-Assessment
Many women with uterine prolapse do not experience symptoms initially. However, as the condition progresses, symptoms such as a feeling of heaviness or fullness in the pelvis, bulging in the vagina, and lower-back pain may occur. It is important for individuals to monitor and assess these symptoms, as they can provide valuable information to healthcare providers. Self-assessment tools and questionnaires may be used to help gauge the severity of symptoms and their impact on daily life. Regular pelvic exams are also crucial for detecting uterine prolapse in its early stages.
The Role of Primary Care and Specialists
When symptoms first start to cause discomfort or interfere with daily activities, it is essential to consult a primary care provider. They can perform initial assessments and refer patients to specialists if necessary. A gynecologist or a urogynecologist, who specializes in female pelvic medicine and reconstructive surgery, may be involved in further evaluation and treatment. These specialists can offer more advanced diagnostic tests and discuss the full range of treatment options available, including non-surgical interventions and surgical procedures.
It is important not to wait until discomfort becomes severe before seeking medical attention. Early diagnosis and treatment can significantly improve quality of life and may prevent the progression of uterine prolapse. If you experience any symptoms of uterine prolapse, or if you have risk factors for the condition, such as a history of multiple vaginal deliveries or menopause, schedule an appointment with your healthcare provider for an evaluation.
Treatment and Management Options
Non-Surgical Interventions
For those experiencing uterine prolapse, a variety of non-surgical interventions can provide relief and prevent further descent of the uterus. Kegel exercises are often recommended to strengthen the pelvic floor muscles. These exercises involve tightening the muscles used to stop urine flow, holding the contraction for several seconds, and then relaxing. It is suggested to perform these exercises in sets throughout the day.
Another non-surgical option is the use of a vaginal pessary, a silicone device inserted into the vagina to support the displaced tissues. Pessaries come in various shapes and sizes and must be regularly removed for cleaning. A healthcare provider can assist in determining the appropriate type and fit of a pessary.
Surgical Treatments
When non-surgical methods are insufficient, surgery may be necessary. Surgical options include hysterectomy, the removal of the uterus, and uterus-sparing procedures for those who may wish to preserve fertility. Additionally, surgeons can repair weak pelvic floor structures with stitches or use synthetic mesh to support vaginal tissues. However, all surgeries carry risks such as bleeding, infection, and the possibility of recurrent prolapse or urinary incontinence. It is crucial to discuss the potential benefits and risks with a healthcare provider.
Lifestyle Adjustments and Home Remedies
Lifestyle changes can alleviate symptoms and reduce the risk of worsening prolapse. Maintaining a healthy weight and a high-fiber diet can prevent constipation and straining during bowel movements. Avoiding heavy lifting and controlling chronic coughing are also beneficial. For smokers, quitting smoking is advised as it can reduce coughing and improve overall tissue health.
Emerging Therapies and Research
Research into new treatments for uterine prolapse is ongoing. Emerging therapies aim to provide more effective and less invasive options for those affected by this condition. Clinical trials are an essential step in the development of new treatments, and participation in such studies can offer access to cutting-edge therapies while contributing to medical research.
It is important to stay informed about the latest research and to consult with a healthcare provider about the possibility of participating in clinical trials or trying new therapies as they become available.

Popular Read
Prevention and Long-Term Outlook
Preventative Measures
The risk of uterine prolapse can be mitigated through several lifestyle and health measures. Regular pelvic floor exercises, such as Kegel exercises, can strengthen the muscles that support the uterus and other pelvic organs. Maintaining a healthy weight is also crucial, as excess body weight can increase the pressure on pelvic structures. Dietary changes that prevent constipation can reduce the strain during bowel movements, which may otherwise weaken pelvic muscles over time. Avoiding heavy lifting and managing chronic coughs or bronchitis can also be beneficial in preventing additional stress on pelvic tissues. Lastly, smoking cessation is advised, as smoking can lead to chronic coughing, contributing to pelvic floor weakening.
Prognosis and Quality of Life
The prognosis for individuals with uterine prolapse varies depending on the severity of the condition and the effectiveness of the treatment. Mild cases may not require treatment and may not significantly impact quality of life. However, moderate to severe cases can cause discomfort, urinary and bowel issues, and sexual dysfunction, which can affect a person’s daily activities and self-esteem. With appropriate treatment, whether non-surgical or surgical, many individuals can expect to see an improvement in symptoms and quality of life. It is important to note that even after successful treatment, there is a possibility of recurrence, especially in those with risk factors such as advanced age or obesity.
Support and Resources
Support for individuals with uterine prolapse is available through various channels. Healthcare providers can offer educational materials and guidance on managing symptoms and improving pelvic floor health. Support groups and online forums can provide a community for sharing experiences and coping strategies. Additionally, physical therapists specializing in pelvic floor rehabilitation can be instrumental in providing personalized exercise programs. For those considering or recovering from surgery, postoperative care teams can offer essential support. It is also beneficial to explore resources provided by professional organizations dedicated to pelvic floor disorders, as they often have the most current information on research and treatment options.