Understanding Lichen Sclerosus
Definition and Overview
Lichen Sclerosus (LS) is a chronic skin condition that predominantly affects the genital and anal areas, leading to the development of thin, white, and patchy skin. While it can occur in men and children, it is more commonly diagnosed in women over the age of 40. LS is not contagious and cannot be spread through intimate contact. The condition can also manifest on other body parts, such as the arms, back, and breasts.
Prevalence and Demographics
LS is considered a rare condition that affects individuals across all racial groups and may have a familial pattern, suggesting a possible genetic component. Although it can affect individuals of any age, it is most prevalent in postmenopausal women, highlighting a potential hormonal influence in its development.
Symptoms and Clinical Presentation
The primary symptoms of LS include significant changes to the affected skin, which becomes thin, dry, and prone to tearing. Patients may experience redness, itching, discomfort, and pain. The skin may develop smooth white patches or become blotchy and wrinkled. In severe cases, the skin may bleed, blister, or form ulcerated sores. When LS affects the genital area, it can lead to painful sexual intercourse or discomfort during urination.
Potential Complications
LS can lead to several complications if left untreated. Persistent inflammation and scarring can cause the vaginal walls to shrink and tighten, which may result in painful sexual intercourse, a condition known as dyspareunia. Additionally, there is an increased risk of developing skin cancer in the affected areas. Early detection and treatment are crucial in managing the symptoms and reducing the risk of cancer.
Etiology of Lichen Sclerosus
Current Theories on Causes
The exact etiology of lichen sclerosus remains elusive, but several theories have been proposed to explain its onset. One prevailing hypothesis suggests that autoimmune mechanisms play a central role, as the condition often coexists with other autoimmune disorders. Another theory points to hormonal imbalances, particularly a deficiency in testosterone and progesterone, which may contribute to the development of the disease. Additionally, chronic irritation or damage to the skin has been implicated as a potential trigger for lichen sclerosus, suggesting that repeated trauma or friction could initiate the inflammatory process.
Risk Factors
While lichen sclerosus can affect individuals of any age and gender, certain risk factors have been identified that increase the likelihood of developing the condition:
- Gender and Age: It is more prevalent in women, particularly those over the age of 40.
- Autoimmune Conditions: Having an autoimmune disorder such as thyroid disease may increase risk.
- Family History: There appears to be a genetic component, as it can run in families.
- Prior Skin Damage: Previous injury or irritation to the affected skin areas may predispose an individual to lichen sclerosus.
Genetic and Environmental Influences
The interplay between genetic predisposition and environmental factors is thought to be significant in the pathogenesis of lichen sclerosus. Genetic susceptibility may be indicated by the familial clustering observed in some cases. However, the exact genetic markers and their mechanisms of action are not fully understood. Environmental influences, such as exposure to certain chemicals or irritants, could act as triggers in genetically predisposed individuals. Moreover, lifestyle factors, including hygiene practices and the use of occlusive clothing, may also contribute to the development of the condition.
In summary, lichen sclerosus is likely the result of a complex interaction between genetic, hormonal, immune, and environmental factors. Understanding these underlying causes is crucial for developing effective prevention strategies and targeted therapies for those affected by this chronic and often painful condition.
Diagnosis of Lichen Sclerosus
Clinical Examination
The initial step in diagnosing lichen sclerosus typically involves a thorough clinical examination by a healthcare provider. During the examination, the provider will look for characteristic signs of the condition, such as white patches, thinning of the skin, and areas of redness or irritation. It is important for patients to report any symptoms they are experiencing, including itching, discomfort, or pain, particularly during sex or when using the bathroom.
Biopsy and Histopathology
If lichen sclerosus is suspected based on the clinical examination, a biopsy may be performed to confirm the diagnosis. This involves removing a small sample of affected tissue and examining it under a microscope. Histopathological analysis can reveal changes in the skin structure that are typical of lichen sclerosus, such as thinning of the epidermis and scarring of the dermis. A biopsy is especially crucial if there is a lack of response to initial treatment or if there is a need to rule out skin cancer, which can be a complication of the condition.
Referral to Specialists
After the initial evaluation, patients may be referred to specialists for further management. These specialists may include dermatologists, who are experts in skin conditions, gynecologists for women’s health concerns, urologists for male patients, and pain medicine specialists if chronic pain is a significant issue. These referrals are important for ensuring a comprehensive approach to treatment and management of lichen sclerosus.
Importance of Early Detection
The importance of early detection of lichen sclerosus cannot be overstated. Early diagnosis and treatment can help manage symptoms, prevent progression of the disease, and reduce the risk of complications, such as scarring and an increased risk of skin cancer. Patients are encouraged to seek medical attention promptly if they notice symptoms suggestive of lichen sclerosus, as early intervention can significantly improve outcomes and quality of life.

⭐️⭐️⭐️⭐️⭐️ “My biggest symptoms are GSM, and because of Mae, they are mostly addressed. I have lived Mae for almost 7 years, and I endorse it all the time.” Margaret C., Damiva Mae Customer
⭐️⭐️⭐️⭐️⭐️ “I’m in my 60’s and post menopause. My doctor recommended I try Damiva MAE, after taking me off hormones (due to developing cysts). I LOVE it. All natural, no hormones, Great vaginal moisturizer. Easy to insert and pleasant smell. So Thankful for MAE.” Paula, Damiva Mae Customer
Treatment Approaches for Lichen Sclerosus
Conventional Treatments
Lichen Sclerosus (LS) is a chronic condition that currently has no cure, but various treatments are available to manage symptoms and prevent complications. The primary goal of conventional treatment is to alleviate itching, reduce soreness, and minimize the risk of scarring. Topical corticosteroids, such as clobetasol ointment, are often the first line of treatment. Initially, the ointment is applied twice daily, and then reduced to twice weekly to prevent symptom recurrence. Regular monitoring for side effects, like further skin thinning, is crucial.
Steroid Creams and Their Limitations
While steroid creams are effective in managing LS symptoms, they come with limitations. Prolonged use can lead to side effects such as skin thinning and increased susceptibility to yeast infections. Therefore, healthcare providers recommend careful application and monitoring. In some cases, a calcineurin inhibitor, like tacrolimus ointment, may be recommended as an alternative to steroids.
Alternative and Complementary Approaches
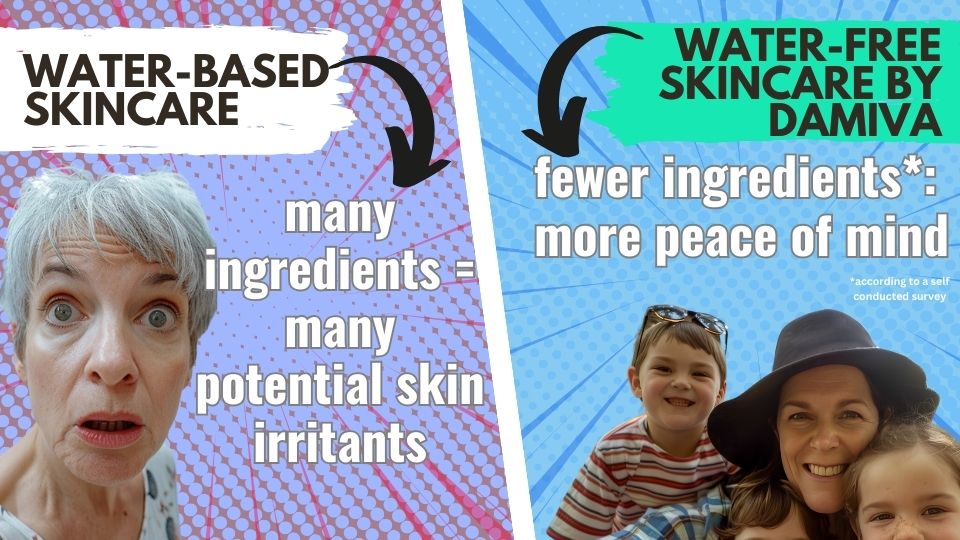
Some patients seek alternative approaches to manage LS symptoms. Water-free and beeswax-free products like Mae by Damiva suppositories and Cleo by Damiva have been reported to provide some moisturizing, soothing and relief from dryness without the side effects associated with steroid creams. These products contain all-natural ingredients and emollient plant butters that promote skin healing and are available without a prescription. However, it’s important to be cautious with alternative approaches and to consult a healthcare provider before use.

⭐️⭐️⭐️⭐️⭐️
“I needed a product like this for medical reasons. Thanks to this product I was able to do my physical therapy. The formula is very comfortable. It provides the right amount of lubrication. I will continue to use. I’m very happy to have found this because nothing else was working.”
Beatriz E, Cleo Customer
Self-Care and Home Remedies
Self-care is an essential aspect of managing LS. Applying vaginal moisturizers can protect the skin, and gentle daily washing with water only or with only mild, unscented soaps can prevent irritation. Taking oral antihistamines at bedtime may help control itching. Additionally, lifestyle modifications such as wearing loose clothing, using unscented toilet paper, and avoiding scented detergents can reduce symptoms. For some, soaking in a lukewarm bath without added products can provide symptom relief.
It’s important for affected women to have regular follow-ups with their healthcare provider to monitor the condition and adjust treatment as necessary. With proper management, many individuals with LS can maintain a good quality of life and minimize the impact of the condition on their daily activities.
Managing Painful Sex Related to Lichen Sclerosus
Impact on Sexual Health
Lichen Sclerosus (LS) is a chronic condition that can significantly affect sexual health. Many women with LS report vulvar pain, which often impacts their quality of life. The condition can lead to changes in the vulva’s architecture, such as scarring and narrowing of the vaginal introitus, resulting in painful sexual intercourse or even preventing penetration altogether. This can cause distress, anxiety, and avoidance of sexual intimacy, further exacerbating the emotional and psychological impact on sexual health.
Therapeutic Interventions
Therapeutic interventions for managing painful sex related to LS include both medical and psychological approaches. Medical treatments primarily involve the use of ultrapotent topical corticosteroids to reduce symptoms and prevent further scarring. However, these treatments may not always result in improved sexual function. Psychosexual counseling has shown significant benefits in improving sexual functioning and quality of life. It includes education about LS, behavioral assignments like sensate focus exercises, desensitization treatment for phobic responses to sexual stimuli, and communication strategies for couples to renegotiate their sexual relationship.
Use of Vaginal Dilators
Vaginal dilators can be an effective tool in managing painful sex for women with LS. Dilators are used to gently stretch the vaginal tissues, which may have become narrowed or less flexible due to LS. The use of dilators can help in reducing pain during intercourse by gradually increasing the capacity of the vaginal canal and promoting tissue elasticity.
Tips for Safe Dilator Use
- Start Slowly: Begin with the smallest dilator size and only progress to larger sizes when comfortable.
- Use Lubrication: Apply a generous amount of water-based lubricant or moisturizer to the dilator to minimize discomfort. Check out these products
- Maintain Hygiene: Always clean the dilator before and after use to prevent infections.
- Be Consistent: Regular use is key to success, but it’s important not to rush the process or force the dilator if experiencing pain.
- Listen to Your Body: If using a dilator causes significant pain, stop and consult with a healthcare provider.
- Prevent UTIs: Urinate immediately after using the dilator to flush out any bacteria that may have been introduced.
It is essential for women with LS to work closely with their healthcare providers to develop a personalized plan for using vaginal dilators safely and effectively.
Prevention and Long-Term Management
Lifestyle Modifications
Living with lichen sclerosus requires adjustments to daily routines to manage symptoms and prevent flare-ups. Patients are advised to:
- Avoid tight clothing that can irritate the skin.
- Avoid products with chemicals or beeswax and use mild, unscented soaps for personal hygiene and avoid over-washing the affected areas.
- Apply emollients like plant butters to protect the skin and maintain moisture.
- Minimize activities that put pressure on the affected areas, such as cycling or horseback riding.
- Manage stress as it can exacerbate symptoms. Techniques such as mindfulness, yoga, or meditation may be beneficial.
Nutritional Support
While there is no specific diet for lichen sclerosus, a balanced diet rich in anti-inflammatory foods may help manage symptoms. Patients should consider:
- Incorporating omega-3 fatty acids found in fish oil supplements and flaxseeds to reduce inflammation.
- Consuming a variety of fruits and vegetables to ensure a high intake of vitamins and antioxidants.
- Avoiding foods that may trigger inflammation, such as processed foods, sugars, and trans fats.
- Staying hydrated to maintain skin elasticity and health.
Regular Monitoring and Follow-Up
Regular check-ups with healthcare providers are crucial for monitoring the progression of lichen sclerosus and adjusting treatment plans as needed. During these visits:
- Patients should report any changes in symptoms or new symptoms.
- Healthcare providers may perform a clinical examination to assess the skin’s condition.
- Follow-up appointments may be scheduled once or twice a year, depending on the severity of the condition.
- Patients should be vigilant for signs of potential complications, such as scarring or changes that might indicate skin cancer.
Early detection and treatment are essential for managing lichen sclerosus effectively. By incorporating lifestyle modifications, nutritional support, and regular medical follow-ups, patients can improve their quality of life and potentially reduce the risk of complications associated with this chronic condition.
Patient Perspectives and Testimonials
Personal Experiences with Treatments
Living with Lichen Sclerosus (LS) can be a challenging journey, and finding the right treatment is often a process of trial and error. Many patients report a moderate level of satisfaction with their treatment, particularly in terms of symptom alleviation. However, it’s not uncommon for individuals to experience frustration when treatments provide only temporary relief or when symptoms recur after cessation of therapy. For some, the use of potent topical steroids has been helpful, significantly reducing itch and improving the integrity of the skin. Others have found success with alternative treatments .
Quality of Life Improvements
The impact of LS on quality of life cannot be overstated. The condition can lead to severe itching, discomfort during sexual intercourse, and sleep disturbances. With effective treatment, many patients report significant improvements in daily functioning and sexual health. The restoration of vulvar architecture through surgical interventions for complications like clitoral phimosis and introital stenosis has also led to enhanced sexual function and satisfaction. Importantly, patients emphasize the value of education and understanding their condition, which empowers them to manage LS more effectively and advocate for their health needs.
Navigating Misinformation
One of the challenges faced by LS patients is the abundance of misinformation surrounding the condition. Misconceptions about the safety of long-term steroid use or the curability of LS can lead to poor treatment adherence and unnecessary anxiety. Patients often benefit from clear communication with healthcare providers who can dispel myths and provide evidence-based information. Support groups and certified dysplasia units have been instrumental in offering reliable advice and fostering a community where patients can share experiences and coping strategies. The role of digital health platforms has also become increasingly important, offering accessible and accurate information to those affected by LS.
In summary, while LS remains a condition without a cure, many women have found relief through personalized treatment plans, surgical interventions, and a supportive care network. The testimonials underscore the importance of patient education, the need for ongoing medical support, and the value of a compassionate approach to managing this chronic condition.