Introduction to Menopause
What is Menopause?
Menopause is a natural biological process that marks the end of a woman’s menstrual cycles and reproductive years. It is diagnosed retrospectively after a woman has gone 12 consecutive months without a menstrual period. This transition typically occurs between the ages of 45 and 56, with the median age being 51 in the United States. Menopause results from the ovaries ceasing to produce significant amounts of estrogen and other reproductive hormones, leading to the end of ovulation and menstruation.
Common Symptoms and Challenges
The journey through menopause can be accompanied by a variety of symptoms and challenges, which can vary significantly among women. Some of the most common symptoms include:
- Vasomotor Symptoms: Hot flashes and night sweats are experienced by approximately 75-80% of women. These can range from mild to severe and can significantly impact daily life and sleep quality.
- Genitourinary Symptoms: Vaginal dryness, burning, and irritation are common due to the thinning of the vaginal mucosa. Urinary symptoms such as frequency and urgency may also occur.
- Psychogenic Symptoms: Many women experience mood swings, irritability, anxiety, and depression. Sleep disturbances, including insomnia and restless leg syndrome, are also prevalent.
- Physical Changes: Weight gain, changes in breast tissue, and a decrease in bone density are common physical changes during menopause.
These symptoms can last for several years and may require various management strategies to improve quality of life.
The Importance of Understanding Hormonal Changes
Understanding the hormonal changes that occur during menopause is crucial for managing its symptoms and associated health risks. The primary hormonal change is the decline in estrogen levels, which affects multiple organ systems. This decline disrupts the hypothalamic-pituitary-ovarian axis, leading to the cessation of ovulation and menstruation.
The reduction in estrogen levels can have several implications:
- Bone Health: Estrogen plays a vital role in maintaining bone density. Its decline can lead to an increased risk of osteoporosis and fractures.
- Cardiovascular Health: Estrogen has protective effects on the cardiovascular system. Lower levels can increase the risk of cardiovascular diseases.
- Mental Health: Estrogen influences mood and cognitive function. Its reduction can contribute to mood swings, depression, and cognitive decline.
By understanding these hormonal changes, women and healthcare providers can better anticipate and manage the symptoms and health risks associated with menopause. This knowledge also underscores the importance of a holistic approach to menopause management, incorporating lifestyle changes, natural remedies, and medical treatments as needed.
The Role of Estrogen in Menopause
Understanding Estrogen
Estrogen is a steroid hormone primarily produced in the ovaries, playing a crucial role in female reproductive health and overall well-being. It is responsible for the development of secondary sexual characteristics, regulation of the menstrual cycle, and maintenance of pregnancy. Estrogen also impacts various non-reproductive functions, including bone density, cardiovascular health, and cognitive function.
There are three main types of estrogen: estrone (E1), estradiol (E2), and estriol (E3). Estradiol is the most potent and prevalent form during the reproductive years, while estrone becomes more dominant post-menopause. Estrogen works by binding to estrogen receptors in various tissues, influencing gene expression and cellular function.
How Estrogen Levels Change During Menopause
Menopause marks the end of a woman’s reproductive years, typically occurring between the ages of 45 and 55. It is characterized by a significant decline in estrogen production due to the depletion of ovarian follicles. This transition is divided into three stages: perimenopause, menopause, and postmenopause.
- Perimenopause: This stage can last several years and is marked by fluctuating estrogen levels. Women may experience irregular menstrual cycles, hot flashes, and other symptoms as estrogen levels become unpredictable.
- Menopause: Defined as the point when a woman has not had a menstrual period for 12 consecutive months. Estrogen levels drop significantly during this time.
- Postmenopause: The period following menopause, where estrogen levels remain consistently low. Symptoms may persist, and the risk of estrogen-related health issues increases.
Impact of Estrogen Deficiency
The decline in estrogen levels during menopause can lead to a variety of symptoms and health concerns:
- Vasomotor Symptoms: Hot flashes and night sweats are common and can significantly impact quality of life. These symptoms result from changes in the hypothalamic regulation of body temperature due to reduced estrogen levels.
- Genitourinary Syndrome: Vaginal dryness, itching, and discomfort during intercourse are prevalent due to the thinning of vaginal tissues. Estrogen deficiency also affects the urinary tract, leading to increased frequency and urgency.
- Bone Health: Estrogen plays a vital role in maintaining bone density. Its deficiency accelerates bone loss, increasing the risk of osteoporosis and fractures.
- Cardiovascular Health: Estrogen has protective effects on the cardiovascular system. Its decline is associated with an increased risk of heart disease and stroke.
- Mental and Emotional Health: Mood swings, anxiety, and depression can occur due to hormonal changes. Estrogen influences neurotransmitter systems that regulate mood and cognition.
In summary, understanding the role of estrogen in menopause is crucial for managing symptoms and mitigating long-term health risks. By recognizing the changes in estrogen levels and their impacts, women can seek appropriate treatments and lifestyle adjustments to improve their quality of life during this transition.
Health Concerns Related to Estrogen Imbalance
Breast Cancer Risks
One of the most significant health concerns related to estrogen imbalance during menopause is the increased risk of breast cancer. Estrogen plays a crucial role in the development and regulation of the female reproductive system, but its influence extends to breast tissue as well. Prolonged exposure to high levels of estrogen has been linked to an increased risk of developing breast cancer. This is particularly concerning for women undergoing hormone replacement therapy (HRT), which often involves the administration of estrogen to alleviate menopausal symptoms.
Studies have shown that the risk of breast cancer increases with the duration of HRT use, especially when combined with progestin. The Women’s Health Initiative (WHI) found that women who took estrogen-progestin therapy had a higher incidence of breast cancer compared to those who did not. However, the risk diminishes after discontinuing the therapy. Therefore, it is crucial for women to discuss the risks and benefits of HRT with their healthcare providers and consider alternative treatments if they have a high risk of breast cancer.
Hormonal Imbalances and Their Effects
Menopause is characterized by a significant decline in estrogen levels, leading to various hormonal imbalances that can affect multiple organ systems. The reduction in estrogen disrupts the delicate balance of hormones that regulate the menstrual cycle, leading to the cessation of menstruation and the onset of menopausal symptoms.
**Vasomotor Symptoms:** Hot flashes and night sweats are among the most common vasomotor symptoms experienced by menopausal women. These symptoms result from the body’s inability to regulate temperature effectively due to fluctuating estrogen levels.
**Genitourinary Syndrome:** Lower estrogen levels can lead to the thinning and drying of vaginal tissues, a condition known as vaginal atrophy. This can cause discomfort during intercourse, increased susceptibility to urinary tract infections, and urinary incontinence.
**Bone Health:** Estrogen plays a vital role in maintaining bone density. Its deficiency during menopause accelerates bone loss, increasing the risk of osteoporosis and fractures. Women may experience a rapid decline in bone mineral density, particularly in the first few years after menopause.
**Cardiovascular Health:** Estrogen has a protective effect on the cardiovascular system by maintaining healthy cholesterol levels and promoting blood vessel flexibility. Its decline can lead to an increased risk of cardiovascular diseases, including heart attacks and strokes.
Mental and Emotional Health
The impact of estrogen deficiency on mental and emotional health is profound and multifaceted. Estrogen receptors are present in various regions of the brain, including those involved in mood regulation and cognitive function. As estrogen levels decline, women may experience a range of psychological symptoms.
**Mood Swings and Depression:** Many women report mood swings, irritability, and feelings of sadness during menopause. The hormonal changes can exacerbate pre-existing mental health conditions or contribute to the onset of new ones. Studies have shown that women in the perimenopausal and early postmenopausal stages are at a higher risk of developing depressive symptoms compared to premenopausal women.
**Anxiety:** Anxiety is another common symptom associated with menopause. The fluctuating hormone levels can lead to increased stress and anxiety, affecting daily life and overall well-being.
**Cognitive Function:** Some women experience cognitive changes during menopause, often referred to as “brain fog.” This can include difficulties with concentration, memory lapses, and a general decline in cognitive sharpness. While these symptoms are usually temporary, they can be distressing and impact work and personal life.
**Sleep Disturbances:** Estrogen deficiency can also lead to sleep disturbances, including insomnia and disrupted sleep patterns. Poor sleep quality can further exacerbate mood disorders and cognitive issues, creating a vicious cycle that affects overall health.
In conclusion, the decline in estrogen levels during menopause can lead to a range of health concerns, from increased breast cancer risks to hormonal imbalances affecting various organ systems, and significant impacts on mental and emotional health. Understanding these risks and working with healthcare providers to manage symptoms can help women navigate this challenging phase of life more effectively.
Natural Solutions for Managing Menopause
Diet and Nutrition
A balanced diet plays a crucial role in managing menopause symptoms. Nutrient-rich foods can help alleviate some of the discomforts associated with this transition. Here are some dietary recommendations:
- Magnesium and Calcium: These minerals are essential for bone health and can help reduce the risk of osteoporosis. Foods rich in magnesium include leafy green vegetables, nuts, and seeds. Calcium can be found in dairy products, fortified plant-based milks, and leafy greens like kale and collards.
- Essential Fatty Acids: Omega-3 fatty acids, found in oily fish such as salmon, mackerel, and sardines, as well as flaxseeds and walnuts, can help manage mood swings and improve overall brain function.
- Phytoestrogens: These plant-based estrogens can mimic the effects of estrogen in the body, potentially reducing hot flashes and night sweats. Foods high in phytoestrogens include soybeans, tofu, flaxseeds, and lentils.
- Vitamin D: This vitamin is crucial for calcium absorption and bone health. Sun exposure and foods like fortified cereals and fatty fish can help maintain adequate levels.
Herbal Remedies
Many women turn to herbal remedies to manage menopause symptoms. While scientific evidence varies, some herbs have shown promise:
- Black Cohosh: This herb is often used to reduce hot flashes and night sweats. However, its effectiveness can vary, and it may not be suitable for everyone, especially those with liver issues.
- Red Clover: Rich in phytoestrogens, red clover may help alleviate hot flashes and improve bone health. Consult with a healthcare provider before use, especially if you have a history of breast cancer.
- Dong Quai: Traditionally used in Chinese medicine, this herb may help balance hormones and reduce hot flashes. However, it can interact with blood thinners, so caution is advised.
- Evening Primrose Oil: Known for its gamma-linolenic acid (GLA) content, this oil may help with hot flashes and breast tenderness. Its effectiveness is still under study, so consult your healthcare provider before use.
Exercise and Physical Activity
Regular physical activity is beneficial for managing menopause symptoms and improving overall health:
- Cardiovascular Exercise: Activities like walking, jogging, swimming, and cycling can help maintain a healthy weight, improve mood, and reduce the risk of heart disease.
- Strength Training: Weight-bearing exercises such as lifting weights or using resistance bands can help maintain bone density and muscle mass, reducing the risk of osteoporosis.
- Flexibility and Balance: Yoga and tai chi can improve flexibility, balance, and mental well-being. These practices can also help reduce stress and improve sleep quality.
- Mind-Body Exercises: Activities like yoga and Pilates combine physical movement with mindfulness, helping to reduce stress and improve overall well-being.
Incorporating these natural solutions into your daily routine can help manage menopause symptoms effectively. Always consult with a healthcare provider before starting any new treatment or supplement to ensure it is safe and appropriate for your individual health needs.

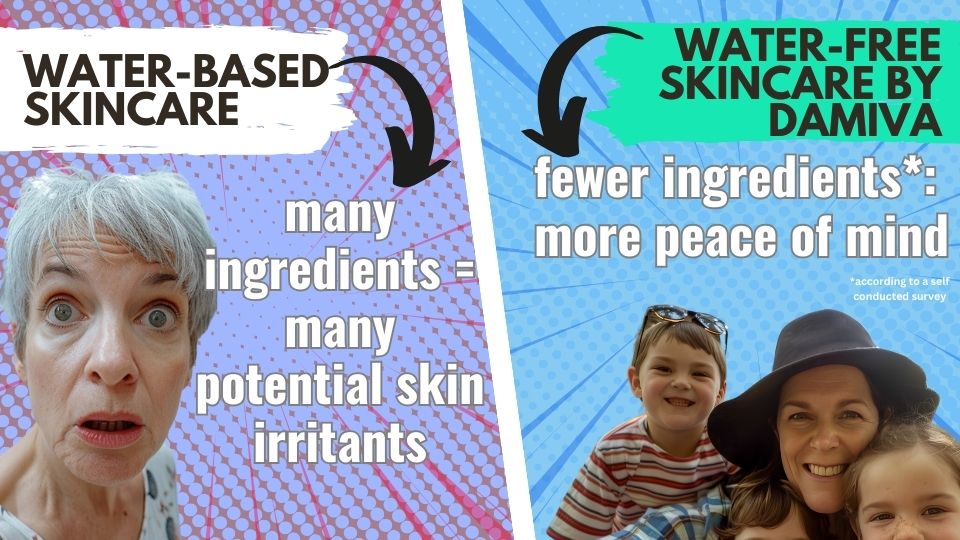
Popular Read: Endocrine Disruptors in Skincare: What You Need to Know
Lifestyle Changes to Support Hormonal Balance
Avoiding Endocrine Disruptors
Endocrine disruptors are chemicals that can interfere with the body’s hormonal systems. These substances are found in a variety of everyday products, including plastics, cosmetics, and pesticides. They can mimic or block hormones and disrupt the body’s normal functions, leading to imbalances that can exacerbate menopausal symptoms.
- Plastics: Avoid using plastic containers for food and drinks, especially those labeled with recycling codes 3 (phthalates), 6 (styrene), and 7 (bisphenols). Opt for glass, stainless steel, or BPA-free plastics instead.
- Cosmetics: Choose personal care products that are free from parabens, phthalates, and synthetic fragrances. Look for labels that indicate the product is free from these chemicals.
- Food: Whenever possible, consume organic produce to reduce exposure to pesticides. Wash fruits and vegetables thoroughly to remove any chemical residues.
- Household Products: Use natural cleaning products and avoid air fresheners and scented candles that may contain harmful chemicals.
Stress Management Techniques
Managing stress is crucial for maintaining hormonal balance, as chronic stress can lead to elevated levels of cortisol, the stress hormone, which can further disrupt other hormonal systems.
- Meditation and Mindfulness: Practicing meditation and mindfulness can help reduce stress levels. Even a few minutes of deep breathing exercises can make a significant difference.
- Physical Activity: Regular exercise, such as yoga, walking, or swimming, can help lower cortisol levels and improve overall mood. Aim for at least 30 minutes of moderate exercise most days of the week.
- Hobbies and Leisure Activities: Engaging in activities that you enjoy, such as reading, gardening, or painting, can provide a mental break and reduce stress.
- Social Support: Spending time with friends and family or joining a support group can provide emotional support and reduce feelings of isolation and stress.
Improving Sleep Quality
Quality sleep is essential for hormonal balance. Poor sleep can disrupt the circadian rhythm and lead to imbalances in hormones such as cortisol, melatonin, and even estrogen.
- Consistent Sleep Schedule: Go to bed and wake up at the same time every day, even on weekends. This helps regulate your body’s internal clock.
- Sleep Environment: Create a sleep-conducive environment by keeping your bedroom cool, dark, and quiet. Consider using blackout curtains and a white noise machine if necessary.
- Limit Screen Time: Avoid screens (phones, tablets, computers) at least an hour before bedtime, as the blue light emitted can interfere with melatonin production.
- Relaxation Techniques: Engage in relaxing activities before bed, such as reading, taking a warm bath, or practicing gentle yoga or stretching.
- Limit Stimulants: Avoid caffeine and alcohol close to bedtime, as they can disrupt sleep patterns.
By making these lifestyle changes, you can support your body’s hormonal balance and alleviate some of the symptoms associated with menopause. These strategies not only help manage menopause but also contribute to overall well-being and health.

Medical and Alternative Treatments
Hormone Replacement Therapy (HRT)
Hormone Replacement Therapy (HRT) is a common treatment for alleviating menopausal symptoms, particularly hot flashes and vaginal discomfort. HRT involves the administration of estrogen or a combination of estrogen and progesterone. Estrogen therapy is typically recommended for women who have had a hysterectomy, while those with an intact uterus are advised to take a combination of estrogen and progesterone to prevent endometrial hyperplasia and cancer.
**Forms of HRT:**
– **Oral Tablets:** Convenient but may have a higher risk of blood clots.
– **Transdermal Patches:** Lower risk of blood clots and liver metabolism issues.
– **Topical Gels and Sprays:** Applied directly to the skin, offering flexibility in dosing.
– **Vaginal Rings, Creams, and Tablets:** Primarily used for treating vaginal and urinary symptoms.
**Benefits:**
– Reduces the frequency and severity of hot flashes.
– Alleviates vaginal dryness and discomfort.
– Helps prevent bone loss and fractures.
**Risks:**
– Increased risk of breast cancer, particularly with long-term use.
– Elevated risk of blood clots and stroke.
– Potential for heart disease if started more than 10 years after menopause.
**Considerations:**
– HRT is most beneficial when started within 10 years of menopause onset and before age 60.
– It should be used at the lowest effective dose for the shortest duration necessary.
Bioidentical Hormones
Bioidentical hormones are chemically identical to those the human body produces. They are derived from plant sources and are often marketed as a more “natural” option compared to traditional HRT. Bioidentical hormones can be custom-compounded in pharmacies based on a healthcare provider’s prescription, although some FDA-approved formulations are available.
**Forms of Bioidentical Hormones:**
– **Compounded Creams and Gels:** Custom-mixed in pharmacies, but lack FDA regulation.
– **FDA-Approved Products:** Available in standardized doses and forms, ensuring quality and safety.
**Benefits:**
– Tailored to individual hormonal needs.
– Perceived as more natural and safer by some women.
**Risks:**
– Lack of regulation and standardization in compounded products can lead to inconsistent dosing and potential safety issues.
– No conclusive evidence that bioidentical hormones are safer or more effective than traditional HRT.
**Considerations:**
– Discuss with a healthcare provider to weigh the benefits and risks.
– Prefer FDA-approved bioidentical hormone products for safety and efficacy.
Acupuncture and Other Alternative Therapies
Alternative therapies offer additional options for managing menopausal symptoms, particularly for women who cannot or prefer not to use hormone-based treatments.
**Acupuncture:**
– Involves the insertion of fine needles into specific points on the body.
– May help reduce the frequency and severity of hot flashes.
– Generally considered safe with minimal side effects.
**Herbal Remedies:**
– **Black Cohosh:** Popular for hot flashes, though evidence of effectiveness is mixed.
– **Soy and Red Clover:** Contain phytoestrogens that may help with mild symptoms.
– **Evening Primrose Oil:** Used for hot flashes, but lacks strong scientific support.
**Mind-Body Practices:**
– **Yoga and Tai Chi:** Improve overall well-being, reduce stress, and may alleviate some menopausal symptoms.
– **Hypnotherapy:** Can help reduce the frequency and intensity of hot flashes.
**Non-Hormonal Medications:**
– **SSRIs and SNRIs:** Antidepressants like paroxetine and venlafaxine can reduce hot flashes.
– **Gabapentin:** Originally for seizures, it can help with hot flashes, especially at night.
– **Clonidine:** A blood pressure medication that may offer mild relief from hot flashes.
**Considerations:**
– Always consult with a healthcare provider before starting any alternative therapy.
– Be aware of potential interactions with other medications and underlying health conditions.
In conclusion, managing menopause effectively often requires a combination of medical and alternative treatments tailored to individual needs and preferences. Consulting with healthcare professionals ensures that the chosen therapies are safe and effective, providing relief from menopausal symptoms while minimizing risks.
Conclusion and Final Thoughts
Summarizing Key Points
Menopause is a natural phase in a woman’s life marked by the cessation of menstrual cycles and a significant decline in estrogen levels. This hormonal shift can lead to a variety of symptoms, including hot flashes, night sweats, mood swings, and vaginal dryness. Understanding the role of estrogen in menopause is crucial for managing these symptoms effectively. Estrogen deficiency can also contribute to long-term health concerns such as osteoporosis and cardiovascular disease.
Several strategies can help manage menopause symptoms and support hormonal balance. Natural solutions include a balanced diet, regular exercise, and herbal remedies. Lifestyle changes, such as avoiding endocrine disruptors, managing stress, and improving sleep quality, can also be beneficial. Medical treatments like Hormone Replacement Therapy (HRT) and bioidentical hormones offer more targeted relief but come with their own set of risks and benefits. Alternative therapies, including acupuncture, provide additional options for those seeking non-pharmacological interventions.
Encouragement for a Holistic Approach
Managing menopause effectively requires a holistic approach that considers both physical and emotional well-being. **Combining natural remedies, lifestyle changes, and medical treatments** can offer a comprehensive strategy for alleviating symptoms and improving quality of life. It’s essential to consult healthcare providers to tailor a personalized plan that addresses individual needs and risk factors.
**Emotional support** is equally important. Menopause can be a challenging time, and having a strong support system can make a significant difference. Engaging in activities that promote mental health, such as mindfulness, yoga, and social interactions, can help manage stress and improve overall well-being.
Resources for Further Support
For those seeking additional information and support, several resources are available:
- The North American Menopause Society (NAMS): Offers comprehensive information on menopause, including treatment options and lifestyle tips. Visit NAMS
- National Institute on Aging: Provides educational materials on menopause and aging. Visit NIA
- Women’s Health Initiative (WHI): A long-term national health study focused on strategies for preventing heart disease, breast and colorectal cancer, and osteoporosis in postmenopausal women. Visit WHI
- Local Support Groups: Many communities offer support groups for women going through menopause. These groups provide a platform to share experiences and coping strategies.
In conclusion, menopause is a significant life transition that requires a multifaceted approach for effective management. By understanding the role of estrogen and exploring various treatment options, women can navigate this phase with greater ease and confidence. Remember, you are not alone—resources and support are available to help you through this journey.