Menopause and Sleep Disturbances
Menopause marks a significant transition in the lives of women, typically occurring between the ages of 45 and 55. It signifies the end of reproductive capability and is characterized by the cessation of menstrual periods. This natural biological process can have profound effects on various aspects of life, including physical health, emotional well-being, and daily functioning. The decline in estrogen and progesterone levels can lead to a range of symptoms, from hot flashes and mood swings to changes in sexual function and bone density.
Common Sleep Problems During Menopause
As women approach menopause, they often experience sleep problems that can significantly affect their quality of life. These issues may include difficulty falling asleep, frequent awakenings during the night, and waking up too early without being able to go back to sleep. The prevalence of such sleep disturbances tends to increase as women transition from perimenopause to postmenopause. Factors contributing to these sleep problems can be multifaceted, encompassing hormonal changes, lifestyle factors, and the presence of menopause-related symptoms such as night sweats.
The Relationship Between Sleep and Menopausal Symptoms
The interplay between sleep and menopausal symptoms is complex and bidirectional. Hormonal fluctuations during menopause can directly impact sleep architecture, leading to less restful sleep and increased awakenings. Conversely, poor sleep can exacerbate menopausal symptoms, creating a challenging cycle of discomfort and restlessness. Hot flashes and night sweats are particularly notorious for disrupting sleep, as they can cause sudden and intense sensations of heat that make it difficult to maintain a comfortable sleep environment. Understanding this relationship is crucial for developing effective strategies to manage sleep disturbances during menopause.
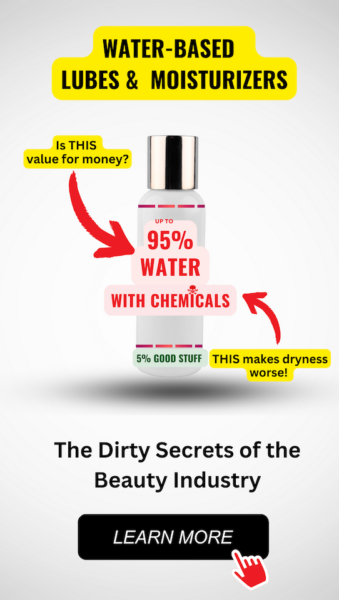
Feeling You Have a Right to Safe Beauty & Fem Care?
If so, it may be time for a change. It starts with knowledge. We have a few suggestions in our new guides.
The Science of Sleep and Menopause
Understanding the Sleep Cycle Changes in Menopause
As women enter the menopausal transition, their sleep patterns often undergo significant changes. The sleep cycle, which includes stages of light sleep, deep sleep, and REM (rapid eye movement) sleep, can become disrupted. During menopause, many women experience a decrease in sleep efficiency, meaning they spend less time in restorative deep sleep and more time awake after initially falling asleep. This can lead to feelings of unrefreshed sleep and daytime fatigue. Additionally, the onset of sleep may take longer, and early morning awakenings become more common, further reducing overall sleep time.
Hot Flashes and Night Sweats: Triggers for Sleep Disruption
Hot flashes and night sweats are hallmark symptoms of menopause that can severely disrupt sleep. These vasomotor symptoms are sudden feelings of intense body heat that can lead to sweating, discomfort, and awakening from sleep. The exact mechanism behind hot flashes is not fully understood, but they are believed to be related to the changes in estrogen levels that affect the body’s temperature regulation. Night sweats, in particular, can cause significant sleep disturbances as they often require women to change clothing or bedding, thereby interrupting sleep and making it difficult to return to a restful state.
The Role of Hormonal Fluctuations in Sleep Quality
Hormonal fluctuations play a critical role in the quality of sleep during menopause. Estrogen and progesterone, two key hormones that regulate the menstrual cycle, also influence sleep architecture. Estrogen is known to have a protective effect on sleep, promoting REM sleep and helping to maintain a lower core body temperature during the night, which is conducive to sleep. Progesterone has a natural sedative effect and can promote sleepiness. As levels of these hormones decline during menopause, women may experience a range of sleep disturbances, including increased sleep latency (time to fall asleep), decreased sleep efficiency, and more frequent awakenings. The interplay between these hormonal changes and sleep is complex, and the impact can vary widely among individuals.
Understanding these changes is crucial for developing strategies to manage sleep problems during menopause. Non-pharmacological approaches, such as maintaining a consistent sleep schedule and creating a sleep-conducive environment, can be beneficial. In some cases, hormone replacement therapy (HRT) may be considered to alleviate severe symptoms. However, it is important to discuss the potential benefits and risks of HRT with a healthcare provider. Ultimately, prioritizing sleep and addressing sleep disturbances proactively can help mitigate the impact of menopause on overall well-being.
By the way, something for you, a little gift!!!
I am just in the middle of publishing my book. It’s about How women can balance their hormones. One part is about food and diet, of course.
Follow this link and enter your email.
I will send you this part of the book for free once the book is published. It has many concrete, practical tips and recipes and will help you feel better during menopause or times of Big hormonal fluctuations.
Annette, Damiva Lead for Health & Wellness

Consequences of Poor Sleep During Menopause
Physical and Emotional Health Impacts
The repercussions of inadequate sleep during menopause extend beyond mere tiredness. A chronic lack of sleep can lead to a host of physical health issues, such as increased blood pressure, weight gain, and a weakened immune system, making it harder to fend off infections. Moreover, there’s a heightened risk of developing more serious conditions like heart disease and diabetes.
Emotionally, the impact is just as profound. Sleep deprivation can exacerbate feelings of anxiety and depression, which are already more prevalent during the menopausal transition. The emotional toll includes increased irritability, mood swings, and a general sense of malaise, which can strain personal and professional relationships.
Cognitive Function and Memory Concerns
As sleep quality deteriorates, so does cognitive performance. Women may notice a decline in concentration, attention, and problem-solving abilities. Memory lapses become more frequent, with research indicating that poor sleep can affect both short-term and long-term memory. This cognitive fog can make it challenging to perform everyday tasks and maintain productivity at work.
Increased Risk of Accidents and Falls
The lack of restorative sleep can lead to a decrease in physical coordination and reaction times, significantly increasing the risk of accidents and falls. This is particularly concerning for menopausal women, as falls can result in serious injuries such as fractures, which may have long-term consequences for mobility and independence. Additionally, the risk of vehicular accidents rises, as drowsy driving is comparable to driving under the influence of alcohol.
In conclusion, the consequences of poor sleep during menopause are far-reaching and can severely impact a woman’s quality of life. It is essential to recognize these potential issues and take proactive steps to manage sleep problems during this transitional period. By doing so, women can mitigate the risks associated with sleep deprivation and maintain their health, well-being, and safety.
Non-Pharmacological Approaches to Improve Sleep
Establishing a Regular Sleep Schedule
Maintaining a consistent sleep schedule is a cornerstone of good sleep hygiene. Going to bed and waking up at the same time every day, even on weekends, helps to regulate your body’s internal clock and can improve the quality of your sleep. Consistency is key, as it reinforces your body’s sleep-wake cycle.
Creating a Restful Sleep Environment
Your bedroom should be a sanctuary for sleep. This means optimizing your environment to enhance sleep quality. Keep the room cool, dark, and quiet, using blackout curtains, eye masks, and earplugs if necessary. Invest in a comfortable mattress and pillows, and consider the use of white noise machines to drown out disruptive sounds. The goal is to make your bedroom a place that signals to your body that it’s time to wind down and rest.
Lifestyle Changes and Bedtime Routines
Lifestyle choices can significantly impact your ability to fall asleep and stay asleep. Avoiding stimulants such as caffeine and nicotine close to bedtime can prevent sleep disruption. Similarly, while alcohol may initially help you relax, it can interfere with your sleep cycle once you’re asleep. Establishing a relaxing bedtime routine can signal to your body that it’s time to wind down. This might include reading, taking a warm bath, or practicing relaxation exercises. Limit exposure to screens before bedtime, as the blue light emitted can interfere with the production of the sleep hormone melatonin.
Do you know the three main ways that your body gets in touch with harmful chemicals with everyday products? Knowledge is Power!
The Ultimate Detox Guide will tell you how to lower your exposure to harmful chemicals!
Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I is a structured program that helps you identify and replace thoughts and behaviors that cause or worsen sleep problems with habits that promote sound sleep. Unlike sleeping pills, CBT-I helps you overcome the underlying causes of your sleep problems. The therapy can help you control or eliminate negative thoughts and worries that keep you awake. It’s typically recommended as the first line of treatment for people with insomnia. CBT-I involves regular visits to a clinician for several weeks and includes practices such as stimulus control therapy and sleep restriction therapy.
These non-pharmacological strategies are not only effective in improving sleep quality but also empower individuals to make sustainable changes that can lead to long-term improvements in sleep and overall health. If you’ve tried these strategies and still struggle with sleep, it may be time to seek professional help.
Medications and Supplements for Sleep Aid
Over-the-Counter Sleep Aids and Their Limitations
Many women experiencing menopause turn to over-the-counter (OTC) sleep aids as a first line of defense against sleep disturbances. These OTC options often include antihistamines, which can induce drowsiness. While they are easily accessible and can be effective in the short term, they come with limitations. One notable drawback is the potential for a “sleep hangover,” a feeling of grogginess the following morning. Additionally, long-term use is not recommended due to the risk of tolerance and dependence. It’s important to consider the timing of these medications to minimize next-day effects and to consult with a healthcare provider if sleep issues persist.
Prescription Medications: Benefits and Risks
When OTC options are insufficient, prescription medications may be considered. These include sedative-hypnotics such as benzodiazepines and non-benzodiazepine hypnotics like Ambien, Sonata, and Lunesta. While these medications can be highly effective in promoting sleep, they must be used with caution due to risks of dependency, cognitive impairment, and diminished efficacy over time. Antidepressants are another class of prescription medications used to address sleep disturbances, particularly when they co-occur with mood disorders. However, it’s crucial to note that some antidepressants may exacerbate insomnia. Hormone therapy may also be an option for those whose insomnia is directly related to menopausal symptoms like night sweats. The decision to use any prescription medication should be made in close consultation with a healthcare provider, considering the individual’s health history and the potential benefits and risks.
The Role of Melatonin and Other Supplements
Melatonin supplements can play a significant role in improving sleep for menopausal women. As a hormone that regulates the sleep-wake cycle, supplemental melatonin may help with sleep onset and quality, especially since melatonin production declines with age. However, it’s essential to source melatonin from reputable suppliers due to variability in actual content versus label claims. Other supplements that may aid sleep include magnolia bark, which can reduce stress and anxiety; L-Theanine, known for promoting relaxation; and magnesium, which is involved in numerous bodily functions including sleep regulation. Additionally, 5-HTP may elevate mood and assist with sleep by increasing serotonin production, while valerian and hops are often used together to improve sleep quality. It’s important to discuss the use of any supplements with a healthcare provider to avoid potential interactions with medications and to ensure they are appropriate for individual health needs.
Medical Disclaimer: The information provided here is for educational purposes only and is not intended as medical advice. Always consult with a healthcare professional before starting any new treatment or supplement regimen.

Bette 100% All-Natural Relaxing Lavender Body Lotion.
Chemical-Free
Your relaxing night time body moisturizer to leave the day’s stress behind. Decompress and wish your body good night with the calming scent of lavender.
When to Seek Professional Help
Identifying When Sleep Problems Need Medical Attention
While occasional sleep disturbances are common during menopause, persistent sleep problems should not be ignored. It’s important to seek medical attention if you experience chronic insomnia, defined as difficulty falling or staying asleep at least three nights a week for three months or more. Additionally, if sleep issues are affecting your daily life, causing you to feel irritable, depressed, or leading to memory concerns, these are signs that professional help may be needed. Other red flags include:
- Regularly waking up feeling unrefreshed despite spending enough time in bed
- Experiencing daytime fatigue or sleepiness that interferes with your daily activities
- Noticing symptoms of sleep apnea, such as snoring or gasping for air during sleep
- Having frequent night sweats that disrupt your sleep and lead to discomfort
Do not hesitate to consult a healthcare provider if you notice these symptoms, as they can also be indicative of other underlying health issues.
What to Discuss with Your Doctor
When you decide to seek help from your doctor, being prepared can make the consultation more effective. Discuss the following:
- Your sleep patterns: Include details such as how long it takes you to fall asleep, how often you wake up at night, and how you feel in the morning.
- Any symptoms you’re experiencing: Mention hot flashes, night sweats, mood changes, or any other menopausal symptoms that could be affecting your sleep.
- Lifestyle habits: Talk about your diet, exercise routine, alcohol and caffeine consumption, and any stressors that might be impacting your sleep.
- Current medications and supplements: Some substances can interfere with sleep, so it’s important to review everything you’re taking.
It’s also beneficial to bring a sleep diary to your appointment, which can provide your doctor with a clearer picture of your sleep issues.
Finding a Trained Therapist for Cognitive Behavioral Therapy
Cognitive Behavioral Therapy for Insomnia (CBT-I) is a highly effective treatment for sleep problems, especially during menopause. To find a trained therapist:
- Ask your doctor for a referral to a therapist who specializes in sleep disorders and has experience with menopausal women.
- Look for certified sleep therapists through reputable organizations such as the American Board of Sleep Medicine or the Society of Behavioral Sleep Medicine.
- Consider online directories of licensed therapists, which often allow you to filter by specialty and insurance acceptance.
CBT-I focuses on changing the thoughts and behaviors that contribute to sleep problems, and a trained therapist can tailor the therapy to address the unique challenges of menopause-related insomnia.
In conclusion, recognizing when to seek professional help is a crucial step towards improving your sleep and overall well-being during menopause. By understanding what to discuss with your doctor and how to find a trained therapist, you can take control of your sleep health and navigate menopause with greater ease.
Additional Resources and Support
Educational Materials and Infographics
Understanding menopause and its impact on sleep is crucial for managing symptoms effectively. A wealth of educational materials is available to help women navigate this transition. The National Institute on Aging (NIA) provides comprehensive guides and infographics that explain the changes occurring during menopause and offer practical tips for improving sleep. These resources can be accessed online and are often available in printable formats, making it easy to share with friends or family members who may also be experiencing similar challenges.
Support Groups and Communities
Support groups offer a space for sharing experiences and advice with others who understand the challenges of menopause-related sleep problems. Online forums and local community groups can be invaluable sources of support. Organizations such as the North American Menopause Society (NAMS) and Women’s Health Concern provide directories of support groups and communities. Participating in these groups can help alleviate feelings of isolation and provide a sense of camaraderie during this phase of life.
Contact Information for Relevant Organizations
For those seeking professional guidance or more detailed information, several organizations specialize in menopause and sleep health. Below is a list of reputable organizations along with their contact information:
- National Institute on Aging (NIA): Offers educational content and research updates. Website: www.nia.nih.gov
- North American Menopause Society (NAMS): Provides a wealth of resources for both healthcare providers and patients. Website: www.menopause.org
- Women’s Health Concern: A patient arm of the British Menopause Society, offering advice and support. Website: www.womens-health-concern.org
- The Sleep Foundation: Offers guidance on sleep health and hygiene. Website: www.sleepfoundation.org
These organizations often provide brochures, contact numbers for helplines, and lists of healthcare providers with expertise in menopause management. They may also offer workshops, webinars, and conferences to educate and empower women dealing with sleep disturbances during menopause.
Remember, while self-education and peer support are valuable, they should complement and not replace professional medical advice. Always consult with a healthcare provider for personalized care and treatment options.









