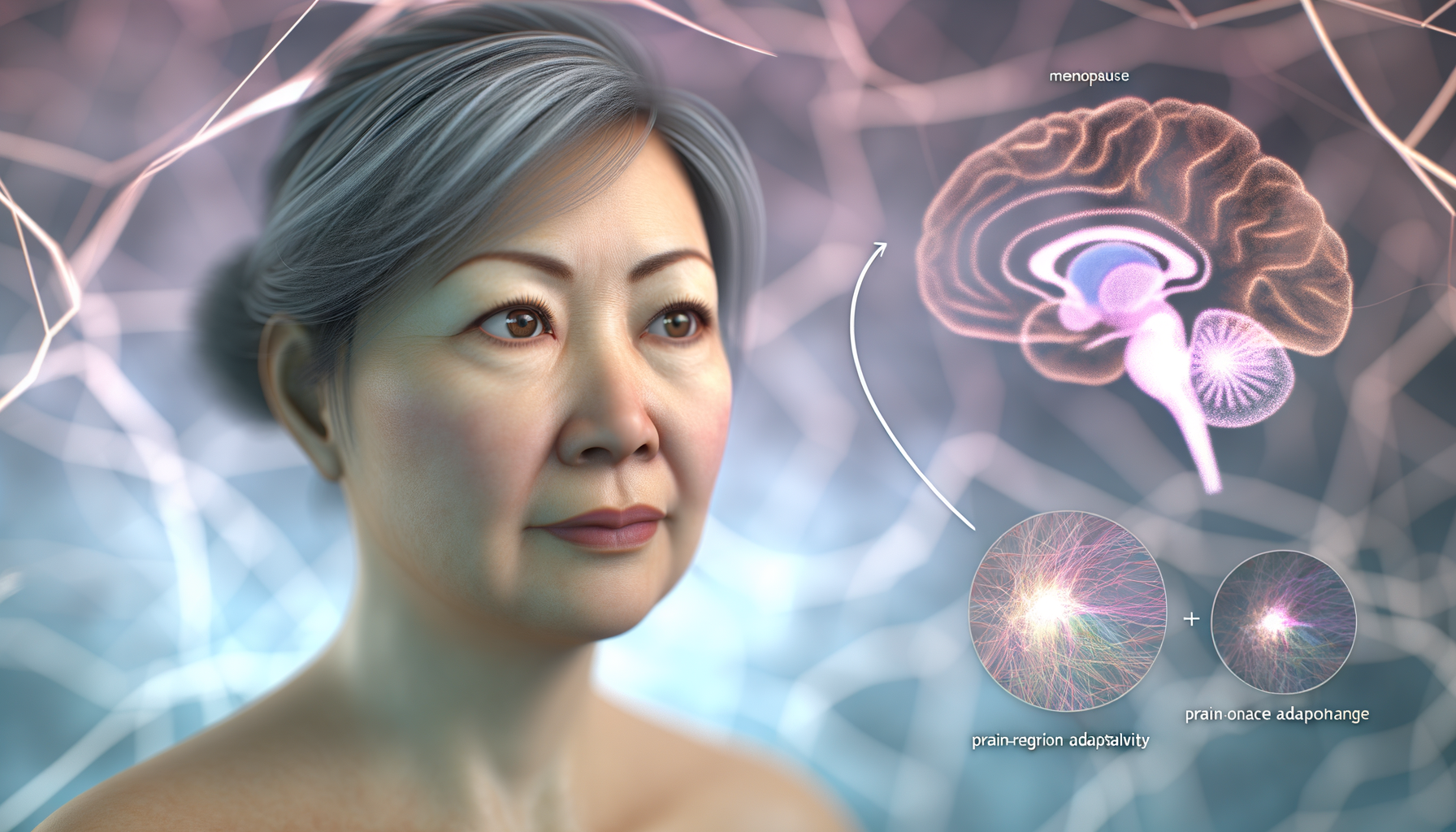
Menopause and Brain Health
Menopause is a natural biological process that marks the end of a woman’s reproductive years. It is clinically defined as the cessation of menstruation for 12 consecutive months, typically occurring during the fifth decade of life. The transition to menopause, known as perimenopause, is characterized by hormonal fluctuations and irregular menstrual cycles. The median age of natural menopause is 51 years, but it can vary due to genetics, lifestyle factors, and health conditions. Surgical menopause, which involves the removal of ovaries via bilateral oophorectomy, leads to a more abrupt decline in hormone production compared to spontaneous menopause.
Estrogen’s Role in Brain Function
Estrogen, a key sex hormone, plays a significant role in brain health and function. It influences cognitive processes, mood regulation, and neuroprotection. Estrogen receptors are found throughout the brain, including areas critical for memory and executive function. The hormone’s decline during menopause has been associated with various neurological symptoms such as memory lapses, mood swings, and changes in cognitive performance. Research suggests that estrogen’s neuroprotective effects may help preserve brain structure and function during the aging process.
Purpose and Significance of the Study
The purpose of this study is to investigate the impact of menopause on brain health by examining changes in brain structure and function during the menopausal transition. The significance lies in understanding how hormonal changes associated with menopause may contribute to cognitive decline and the increased risk of neurodegenerative diseases such as Alzheimer’s. This research aims to provide insights into potential interventions, such as hormone therapy, that could mitigate the adverse effects of menopause on brain health. Additionally, the study seeks to inform healthcare providers and women about the importance of monitoring brain health during this critical life stage.
Methodology of the Brain Imaging Study
Participant Demographics
The study enrolled 182 cognitively intact women aged 40–65 years. After exclusions due to neuropathological conditions, artifacts, incomplete clinical data, and unclear menopause status, the final sample consisted of 161 participants. This included 30 pre-menopausal (PRE), 57 peri-menopausal (PERI), and 74 post-menopausal (POST) women. The demographic and clinical measures were comparable across groups, except for age differences between PRE and POST groups. To address age effects, analyses included age as a confounder and comparisons with age-matched male groups. The distribution of APOE-4 carriers, a genetic risk factor for Alzheimer’s disease, was also comparable between groups.
Imaging Techniques Used
The study employed a multi-modality neuroimaging approach, including:
- Magnetic Resonance Imaging (MRI): Used to assess gray matter volume (GMV) and white matter volume (WMV).
- MRI-Diffusion Tensor Imaging (DTI): Provided fractional anisotropy (FA) measurements, indicating white matter integrity and structural connectivity.
- 18F-fluorodeoxy-2-glucose Positron Emission Tomography (FDG-PET): Measured cerebral glucose metabolism (CMRglc).
- Arterial Spin Labeling (ASL): Estimated cerebral blood flow (CBF).
- 31 Phosphorus-Magnetic Resonance Spectroscopy (31P-MRS): Assessed ATP production.
- 11C-Pittsburgh compound B (PiB) PET: Quantified amyloid-beta (Aβ) deposition.
These techniques were selected for their ability to provide comprehensive data on brain structure, connectivity, energy metabolism, and pathological protein accumulation.
Parameters and Measures for Analysis
The study’s primary outcomes were changes in brain biomarkers across menopausal stages. The parameters and measures for analysis included:
- Structural Biomarkers: Differences in GMV and WMV, with a focus on regions involved in higher-order cognitive functions.
- Metabolic Biomarkers: Variations in CMRglc, CBF, and ATP production, particularly in temporo-parietal regions.
- Aβ Deposition: Increased PiB uptake as an indicator of AD risk, with special attention to APOE-4 carriers.
Statistical analysis was adjusted for age, APOE-4 status, and modality-specific confounders. Voxel-based results were significant at p < 0.05, cluster-level corrected for family-wise type error (FWE). The study also included longitudinal follow-up scans to examine persistence of biomarker effects post-menopause.
By employing this rigorous methodology, the study aimed to elucidate the complex changes occurring in the brain during the transition to menopause, providing valuable insights into the neurological underpinnings of this critical life stage.
Findings on Brain Structure Changes
Gray Matter Volume Variations
One of the most significant findings from the imaging study was the observation of gray matter volume (GMV) variations across different stages of menopause. The inferior temporal gyrus, a region associated with high-level visual perception, exhibited a notable decrease in GMV from pre-menopausal to post-menopausal women. This reduction in gray matter was not uniform across the brain but was particularly pronounced in areas linked to memory and perception. Interestingly, a temporary dip in GMV was also noted in the precuneus during the peri-menopausal phase, which appeared to resolve post-menopause, suggesting a transient restructuring of brain matter during this transition.
White Matter Volume Changes
Alongside alterations in gray matter, the study also documented changes in white matter volume (WMV). Multiple regions throughout the brain, including the anterior and posterior corona radiata, showed a decline in WMV in post-menopausal participants compared to their pre-menopausal counterparts. These findings indicate that the menopause transition affects not only the neuron cell bodies but also the connective nerve fibers that facilitate communication between different brain regions.
Regional Brain Alterations
The imaging techniques used in the study allowed for a detailed analysis of regional brain alterations. In addition to the aforementioned changes in the inferior temporal gyrus and precuneus, other areas such as the fusiform gyrus and supramarginal gyri also exhibited variations in response to menopause. The study’s comprehensive approach revealed that these alterations are not merely a result of chronological aging but are specifically associated with the hormonal and neuroendocrine changes that characterize the menopause transition.
In summary, the imaging study provided valuable insights into the structural reorganization of the female brain during menopause. The observed changes in gray and white matter volumes, as well as the regional brain alterations, underscore the complex interplay between hormonal fluctuations and brain structure. These findings contribute to a better understanding of the neurological aspects of menopause and pave the way for future research on the implications of these brain changes for cognitive function and overall brain health.
Brain Function and Metabolism During Menopause
Cerebral Blood Flow and Glucose Consumption
The menopausal transition, marked by a significant decline in estrogen production, brings about notable changes in cerebral blood flow (CBF) and glucose consumption within the brain. Estrogen is known to play a crucial role in the regulation of both these factors, which are vital for maintaining cognitive function and overall brain health. As women transition from pre-menopause to post-menopause, studies have observed a decline in the utilization of glucose in various regions of the brain, particularly in the temporal lobes, which are associated with memory and perception. This reduction in glucose metabolism suggests a decrease in neuronal activity and energy demand.
However, the brain appears to initiate compensatory mechanisms to counteract these declines. Increases in cerebral blood flow have been documented in the same regions experiencing reduced glucose consumption. This suggests that the brain may be attempting to maintain energy balance and support neuronal function despite the reduction in primary fuel availability. The precise mechanisms behind these compensatory increases in blood flow are not yet fully understood, but they may involve upregulation of other metabolic pathways or changes in vascular responsiveness.
ATP Production and Brain Energy Utilization
Adenosine triphosphate (ATP) is the primary energy currency of the cell, and its production is essential for all cellular functions, including those in neurons. During menopause, the brain’s energy utilization patterns undergo significant changes. Despite a decrease in glucose consumption, ATP production in the brain does not necessarily decline. In fact, some studies have reported increases in ATP production post-menopause, particularly in brain regions that also show increased cerebral blood flow.
This suggests that the brain may adapt to the reduced availability of glucose by enhancing the efficiency of ATP production or by utilizing alternative energy substrates. The maintenance or increase in ATP levels could be a critical factor in preserving cognitive function during and after the menopausal transition. It is also indicative of the brain’s remarkable plasticity and its ability to adapt to changing hormonal environments.
Transient vs. Persistent Functional Changes
Not all changes in brain function and metabolism during menopause are permanent. Some alterations appear to be transient, occurring during the peri-menopausal period and then reversing or stabilizing once menopause is complete. For instance, temporary dips in gray matter volume in regions such as the precuneus, which is involved in memory and self-awareness, have been observed to resolve post-menopause.
Similarly, changes in white matter volume and glucose utilization have been noted to partially stabilize or even reverse in the years following menopause. This suggests that while the menopausal transition can temporarily disrupt brain function, there is potential for recovery and return to a new homeostatic baseline. The brain’s ability to recover and adapt is associated with improved memory and cognitive performance, highlighting the resilience of the female brain during this period of significant hormonal change.
Understanding the distinction between transient and persistent changes is crucial for developing targeted interventions to support brain health in menopausal women. It also underscores the importance of longitudinal studies to track brain function over time and to differentiate between the effects of menopause and those of normal aging.
In conclusion, the transition to menopause is a period of significant change for brain function and metabolism. Despite challenges posed by reduced estrogen levels, the brain exhibits a remarkable capacity for adaptation, maintaining cognitive function through a variety of compensatory mechanisms. These findings not only enhance our understanding of the menopausal transition but also provide hope for interventions that can support women’s brain health during this critical period.

Cognitive Implications and Compensatory Mechanisms
Brain Adaptations to Menopausal Changes
The menopause transition (MT) is a period of significant neuroendocrine change that affects various organ systems, including the brain. During this transition, the decline in sex hormones, particularly 17β-estradiol, has a broad impact on neural processes. These changes are reflected in alterations in gray matter volume (GMV), white matter volume (WMV), and brain energy metabolism. Notably, cognition is preserved post-menopause, which correlates with GMV recovery and brain adenosine triphosphate (ATP) production, suggesting potential compensatory mechanisms at play.
Impact on Memory and Cognitive Performance
Studies have shown that menopausal status is associated with changes in memory and cognitive performance. For instance, post-menopausal women often report memory lapses and cognitive difficulties. Imaging analyses have reported declines in glucose metabolism and GMV in post-menopausal women, which were modulated by hormone treatment (HT), indicating dynamic neuro-endocrine processes well into menopause. However, despite these changes, cognitive performance, particularly memory function, tends to be maintained post-menopause. This preservation of cognition has been linked to structural brain adaptations and increased ATP production in the brain, highlighting the brain’s ability to compensate for hormonal changes.
Comparison with Male Aging Patterns
When comparing each MT group to an age-matched male group, results indicated that MT-stage effects on biomarkers were specific to menopausal endocrine aging rather than chronological aging. For example, both post- and peri-menopausal groups exhibited lower GMV in several cortical regions and subcortical structures compared to males. However, GMV generally stabilized post-menopause and selectively recovered in regions such as the precuneus. This suggests that the female brain undergoes a unique pattern of structural changes and adaptations during the MT that differ from male aging patterns.
Menopause, Alzheimer’s Risk, and Genetic Factors
Menopause has been linked to an increased risk of Alzheimer’s disease (AD), particularly in women carrying the apolipoprotein epsilon-4 genotype (APOE-4). The MT, especially the peri-menopause stage, is associated with lower GMV, hypometabolism, and emerging amyloid-beta (Aβ) deposition, which are hallmarks of AD. This increased deposition of Aβ in peri- and post-menopausal women, especially among APOE-4 carriers, indicates a specific risk for AD with onset in the peri-menopause. However, it is important to note that reproductive aging is not uniformly associated with AD risk, and more studies are needed to understand the complex relationships between MT, brain aging, and genetic factors.
The findings from various studies suggest that the MT is a dynamic neurological process that reshapes the neural landscape of the female brain during midlife endocrine aging. The brain’s ability to adapt structurally and bioenergetically to the hypo-estrogenic post-menopausal state may account for the preservation of cognitive function post-menopause. These adaptations may include increased GMV in associative cortical areas and enhanced ATP production. Additionally, the presence of Aβ deposition in peri- and post-menopausal women, particularly among APOE-4 carriers, highlights the need for further research to clarify the role of menopause in AD risk and to identify factors that impact successful brain adaptation post-menopause.

THEN IT CONTAINS TOXIC CHEMICALS. WHY RISK IT GETTING SICK? GO CHEMICAL FREE.
Menopause, Alzheimer’s Risk, and Genetic Factors
Amyloid Beta Plaque Accumulation
The menopausal transition is marked not only by endocrine changes but also by significant shifts in brain structure and function. One of the most concerning changes observed is the accumulation of amyloid beta (Aβ) plaques, which are closely associated with Alzheimer’s disease (AD). During menopause, the decline in estrogen—a hormone with protective effects on the brain—has been linked to an increase in the deposition of these plaques. This connection is particularly evident in women carrying the apolipoprotein E epsilon-4 (APOE ε4) allele, a known genetic risk factor for late-onset AD. The accumulation of Aβ plaques in peri- and post-menopausal women, especially those with the APOE ε4 variant, underscores the potential role of menopause as a critical period for interventions aimed at reducing Alzheimer’s risk.
Influence of APOE ε4 Variant
The APOE ε4 allele is the most significant genetic risk factor for late-onset Alzheimer’s disease. Research has shown that peri- and post-menopausal women who are carriers of the APOE ε4 allele have a higher propensity for Aβ plaque accumulation compared to their non-carrier counterparts. This genotype appears to exacerbate the risk of Alzheimer’s during the menopausal transition, suggesting a gene-hormone interaction that could be pivotal in understanding gender disparities in AD prevalence. The influence of the APOE ε4 variant on amyloid accumulation during menopause highlights the importance of personalized medical approaches that consider genetic profiles.
Gender Differences in Alzheimer’s Risk
Women are disproportionately affected by Alzheimer’s disease, representing over two-thirds of those diagnosed. The menopausal transition has emerged as a potential explanation for this gender disparity. Unlike the gradual age-related cognitive decline observed in men, women experience a more pronounced shift in brain biomarkers during menopause, which may contribute to their increased vulnerability to AD. The interplay between genetic factors, such as the presence of the APOE ε4 allele, and the hormonal upheaval of menopause could be key to understanding why women are at greater risk. Recognizing these gender differences is crucial for developing targeted strategies to mitigate Alzheimer’s risk in women.
Overall, the menopausal transition represents a window of increased vulnerability for women, with changes in brain structure and function that may predispose them to Alzheimer’s disease. The interaction between genetic factors like the APOE ε4 variant and the decline in estrogen during menopause underscores the need for further research and potential interventions tailored to women’s health.
Do you know the three main ways that your body gets in touch with harmful chemicals with everyday products? Knowledge is Power!
The Ultimate Detox Guide will tell you how to lower your exposure to harmful chemicals!

Conclusions and Implications for Women’s Health
Reshaping the Female Brain Post-Menopause
The transition to menopause is a significant physiological event that can reshape the landscape of the female brain. Research has shown that the steep decline in estrogen production during menopause is associated with changes in brain structure, function, and metabolism. However, the brain demonstrates a remarkable ability to adapt to these changes. Studies using MRI and PET scans have revealed that, despite reductions in gray matter volume and glucose metabolism, the brain can compensate with increased cerebral blood flow and ATP production. This compensatory mechanism is thought to help maintain cognitive function despite the hormonal changes that occur during menopause.
Overcoming the Stigma of Menopause
Menopause has historically been stigmatized and associated with negative stereotypes, particularly around cognitive decline. However, emerging imaging studies emphasize that menopause is a normal part of aging and that the brain is capable of finding a new “normal” after this transition. By disseminating these findings, healthcare providers and society at large can help to overcome the stigma surrounding menopause, encouraging women to approach this phase of life with confidence and to seek support and care when needed.
Future Directions and Preventative Care
As we continue to unravel the complexities of the brain’s response to menopause, it is crucial to focus on preventative care and early intervention strategies. Future research should explore the long-term cognitive implications of menopausal brain changes and investigate potential protective factors, such as lifestyle modifications and hormone replacement therapy. Additionally, personalized medicine approaches that consider genetic factors, such as the APOE ε4 variant, could offer more tailored strategies for maintaining brain health during and after the menopausal transition.
Ultimately, the goal is to empower women with the knowledge and resources to take proactive steps in preserving their cognitive health, ensuring a high quality of life as they age.