Menopause marks a significant transition in a woman’s life, typically occurring in the late 40s to early 50s, signifying the end of menstrual cycles and reproductive fertility. It is defined by the cessation of menstruation for one continuous year. Menopause is a natural biological process, not a medical illness, but it can lead to various physical and emotional symptoms as the body adjusts to decreasing levels of estrogen and progesterone. The significance of menopause lies not only in its physical manifestations but also in its psychological and social implications, as it often coincides with other life transitions.
Common Misconceptions and Knowledge Gaps
Despite being a universal female experience, menopause is shrouded in misconceptions. A common misunderstanding is that menopause occurs abruptly, while in reality, it is a gradual process. Another knowledge gap is the belief that menopause only causes physical symptoms like hot flashes and night sweats, ignoring the emotional and cognitive changes many women face. Additionally, the idea that menopause leads to a decline in sexuality is a misconception; many women continue to enjoy an active sex life post-menopause. Understanding these misconceptions is crucial for demystifying menopause and empowering women with accurate information.
Overview of Menopause Stages
Menopause unfolds in three stages, each with distinct characteristics and symptoms. Perimenopause is the precursor to menopause, where hormonal fluctuations begin, and women may start experiencing irregular menstrual cycles and symptoms such as hot flashes. This stage can last several years. Menopause itself is the point at which a woman has not had a menstrual period for 12 months; it is during this time that symptoms can intensify. Finally, postmenopause is the phase following menopause, where symptoms may ease for many, but long-term health risks associated with lower estrogen levels, such as osteoporosis and heart disease, may emerge. Understanding these stages helps women anticipate changes in their bodies and seek appropriate care and support.
Understanding Hormonal Changes
Role of Estrogen and Progesterone
Estrogen and progesterone are the primary hormones that regulate a woman’s menstrual cycle and play a significant role in her reproductive system. Estrogen is responsible for the development of secondary sexual characteristics and the thickening of the uterine lining during the menstrual cycle. Progesterone prepares the uterus for potential pregnancy after ovulation and moderates the effects of estrogen. During menopause, the levels of these hormones fluctuate and eventually decline, leading to the cessation of menstrual periods and the end of fertility.
How Hormonal Fluctuations Affect the Body
The hormonal fluctuations that occur during menopause can have a wide range of effects on the body. As estrogen levels decrease, women may experience vasomotor symptoms such as hot flashes and night sweats. Other common symptoms include vaginal dryness, decreased libido, and changes in mood. The decline in estrogen can also lead to longer-term health issues, such as osteoporosis, due to its role in maintaining bone density. Additionally, hormonal changes can affect bladder control and the health of the bladder and urethra lining, leading to urinary incontinence. These changes can significantly impact a woman’s quality of life and overall well-being.
The Biological Process of Ovarian Egg Depletion
Menopause is a biological process that is marked by the depletion of ovarian eggs. A woman is born with a finite number of eggs, which are stored in the ovaries. The ovaries also produce estrogen and progesterone, which control menstruation and ovulation. Menopause occurs when the ovaries no longer release an egg every month and menstruation stops. This process is gradual and is preceded by perimenopause, where hormone production becomes erratic and menstrual cycles become irregular. Eventually, the ovaries cease to function, and the body enters menopause, followed by postmenopause, which marks the end of ovarian hormonal production and the permanent cessation of menstrual periods.
Understanding these hormonal changes is crucial for women as they approach menopause. It allows them to anticipate the changes in their bodies and seek appropriate treatment and support. By recognizing the symptoms and effects of hormonal fluctuations, women can better manage their health during this transition.
Feeling You Have a Right to Safe Beauty & Fem Care?
If so, it may be time for a change. It starts with knowledge. We have a few suggestions in our new guides.
Perimenopause: The Menopause Precursor
Early Signs and Symptoms
Perimenopause marks the transition leading up to menopause, where the body begins to exhibit changes signaling the end of reproductive years. Early signs and symptoms of perimenopause can vary widely among women but commonly include irregular periods, hot flashes, vaginal dryness, urinary urgency, and sleep problems. Many women also experience mood changes such as increased anxiety, depression, or irritability. Physical changes may include weight gain, decreased muscle mass, and the development of facial hair due to hormonal imbalances. Cognitive changes, such as difficulty concentrating and minor memory problems, are also reported.
Duration and Variability of Perimenopause
The duration of perimenopause can be quite variable, typically lasting anywhere from a few months to several years. Most women begin to notice perimenopausal symptoms in their 40s, but the onset can occur earlier. The variability is influenced by factors such as genetics, lifestyle, and overall health. Smoking, for example, has been associated with an earlier onset of menopause.
Early vs. Late Menopause Transition
The menopause transition can be divided into early and late stages. The early stage is characterized by more subtle changes in menstrual cycle length and hormonal fluctuations, while the late stage is marked by more pronounced symptoms and greater irregularity of periods. It is important to note that while fertility decreases during this time, pregnancy is still possible until menopause is confirmed, which is defined as 12 consecutive months without a menstrual period.
Managing Symptoms and Lifestyle Adjustments
Managing the symptoms of perimenopause often requires a combination of lifestyle adjustments and medical interventions. Lifestyle strategies include regular exercise, maintaining a healthy diet, ensuring adequate sleep, and engaging in mentally stimulating activities to combat cognitive changes. Non-hormonal treatments such as vaginal lubricants can alleviate vaginal dryness, and various medications may be prescribed to manage mood swings and hot flashes.
It is also crucial for women to have open discussions with their healthcare providers about their symptoms and treatment options. Emotional support from counseling or support groups can be beneficial during this transition. For those experiencing significant symptoms, hormone therapy may be considered, but it requires a thorough evaluation of the benefits and risks by a healthcare professional.

Navigating Through Menopause
Identifying the Transition to Menopause
The journey into menopause, often beginning in a woman’s 40s, is marked by the transition phase known as perimenopause. This stage is characterized by the body providing physical clues that the menopause process is underway, potentially years before menstruation ends. Irregular periods, hot flashes, vaginal dryness, sleep disturbances, and mood swings are common signs due to fluctuating ovarian hormones, particularly estrogen. It’s important to note that menopause is confirmed after a woman has not had her period for 12 consecutive months.
Common Symptoms and Their Intensity
Menopause symptoms vary widely among women, but the most prevalent include hot flashes, night sweats, vaginal atrophy, and mood changes. While some women may experience mild discomfort, others face more severe and disruptive symptoms. Hot flashes can be particularly intense, often accompanied by increased heart rate and sweating. Psychological symptoms such as anxiety, depression, and irritability can also be significant, impacting mental health and quality of life.
Approaches to Alleviate Discomfort
Managing menopause symptoms can involve a variety of strategies. Lifestyle adjustments such as layered clothing, dietary changes, and stress reduction can help mitigate hot flashes. Regular exercise and a balanced diet support overall health and may alleviate some symptoms. Additionally, non-hormonal treatments and alternative therapies like herbal supplements or acupuncture have been explored by some women seeking relief.
When to Seek Medical Advice
While many menopause symptoms can be managed with lifestyle changes and self-care, it’s crucial to seek medical advice when symptoms become unmanageable or severely impact daily life. Healthcare providers can offer guidance on hormone therapy, which has been shown to relieve discomfort for many women, though it comes with its own set of risks and benefits. Women experiencing symptoms of menopause should have open discussions with their healthcare providers to determine the best individualized treatment plan.
Do you know the three main ways that your body gets in touch with harmful chemicals with everyday products? Knowledge is Power!
The Ultimate Detox Guide will tell you how to lower your exposure to harmful chemicals!

Postmenopause: Life After Menopause
Changes in Symptoms Post-Menopause
After the cessation of menstrual periods for over a year, women enter the postmenopausal phase. While some may continue to experience menopausal symptoms such as hot flashes and mood swings, others may notice a significant reduction or complete end to these symptoms. However, the hormonal changes that characterize menopause do not reverse, and the body adjusts to a new normal with consistently low levels of estrogen and progesterone.
Long-Term Health Risks and Prevention
The decline in estrogen levels post-menopause can lead to increased risks for several health conditions. Cardiovascular disease becomes a more significant concern as estrogen’s protective effects on heart and artery health diminish. To combat this, women are encouraged to maintain a healthy diet, exercise regularly, and avoid smoking. Osteoporosis is another major risk due to accelerated bone density loss. Preventative measures include consuming calcium-rich foods, taking supplements as needed, and engaging in weight-bearing exercises. Vaginal atrophy and urinary tract changes also pose challenges, with vaginal lubricants and topical creams being helpful for dryness and discomfort.
The Importance of Ongoing Health Monitoring
Continued health monitoring is crucial in the postmenopausal years. Regular check-ups with healthcare providers can help in the early detection and management of the aforementioned health risks. Women should undergo bone mineral density testing to assess the risk of osteoporosis, blood pressure and cholesterol checks for heart health, and screenings for cancers that are more prevalent in postmenopausal women, such as breast and ovarian cancer. Additionally, addressing any mental health concerns with a professional is important, as mood changes can persist or emerge during this stage.
By understanding the changes that occur post-menopause and taking proactive steps in health management, women can maintain a high quality of life and mitigate the risks associated with this natural phase of aging.
Treatment and Management Strategies
Holistic and Lifestyle Approaches
Adopting a holistic and lifestyle-centered approach can be beneficial in managing menopause symptoms. Regular physical activity and a balanced diet are foundational to maintaining overall health and can help mitigate weight gain and mood swings. Stress-reduction techniques such as yoga, meditation, and deep-breathing exercises can alleviate anxiety and improve sleep quality. Additionally, engaging in mentally stimulating activities and maintaining social connections can help address concentration and memory concerns. It’s important to note that while over-the-counter supplements like St. John’s wort or vitamin B6 are popular, they should only be used under the guidance of a healthcare provider to avoid potential side effects.
Hormone Therapy: Benefits and Considerations
Hormone therapy (HT), also known as hormone replacement therapy (HRT), involves the administration of estrogen and, if the uterus is intact, progesterone. This treatment can effectively reduce vasomotor symptoms such as hot flashes and night sweats and help prevent osteoporosis. However, HT is not suitable for everyone; it is contraindicated in individuals with a history of certain cancers, blood clots, liver disease, stroke, or those who may be pregnant. The decision to use HT should be made after a thorough discussion with a healthcare provider, considering the individual’s medical history and symptom severity.
Non-Hormonal Treatment Options
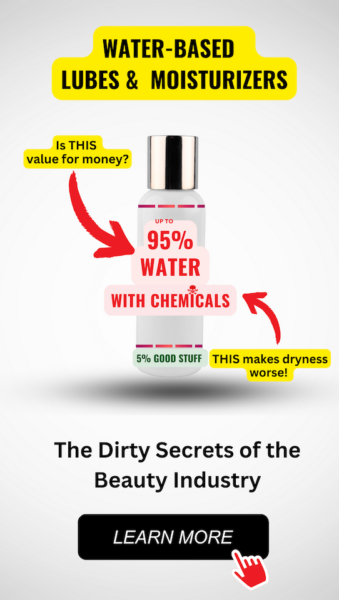
For those who cannot or choose not to use hormone therapy, non-hormonal medications can offer relief. Selective serotonin reuptake inhibitors (SSRIs), typically used to treat depression, can also alleviate hot flashes and mood changes. Other options include antiseizure drugs and blood pressure medications. For vaginal dryness and discomfort during intercourse, water-soluble lubricants and vaginal moisturizers can be effective. Regular sexual activity can also help maintain vaginal health by promoting blood flow to the genital area.
Customizing Treatment Based on Individual Needs
Menopause is a highly individual experience, and treatment should be tailored to each person’s unique needs. A healthcare provider can help determine the most appropriate interventions, which may include a combination of lifestyle changes, hormone therapy, and non-hormonal treatments. It’s crucial for individuals to communicate openly with their healthcare providers about their symptoms and how they affect their quality of life. Together, they can develop a personalized management plan that addresses both immediate discomfort and long-term health considerations.
Remember: Always consult with a healthcare provider before starting any new treatment to ensure it is safe and appropriate for your specific health situation.
By the way, something for you, a little gift!!!
I am just in the middle of publishing my book. It’s about How women can balance their hormones. One part is about food and diet, of course.
Follow this link and enter your email.
I will send you this part of the book for free once the book is published. It has many concrete, practical tips and recipes and will help you feel better during menopause or times of Big hormonal fluctuations.
Annette, Damiva Lead for Health & Wellness

Conclusion: Empowering Women Through Menopause Education
The Importance of Open Dialogue with Healthcare Providers
One of the most critical aspects of navigating menopause is the establishment of an open and honest dialogue with healthcare providers. Women should feel empowered to discuss their symptoms, concerns, and treatment options without fear of judgment or dismissal. Healthcare professionals play a pivotal role in demystifying menopause and providing accurate information that can alleviate fears and misconceptions. By fostering a supportive environment, healthcare providers can encourage women to actively participate in their care, leading to more personalized and effective management of menopausal symptoms.
Advocating for Personalized Care
Menopause is a highly individual experience, with symptoms and their intensity varying greatly among women. It is essential that treatment and management strategies are tailored to each woman’s unique needs. Personalized care requires a comprehensive understanding of a woman’s health history, lifestyle, and preferences. Women should be encouraged to advocate for themselves, ensuring that their voices are heard and their concerns are addressed. This personalized approach not only improves the quality of care but also enhances the overall well-being of women during this transition.
Resources and Support for Women Experiencing Menopause
Access to resources and support is vital for women undergoing menopause. Educational materials, support groups, and community-based interventions can provide women with the knowledge and tools needed to manage their symptoms effectively. These resources can also offer psychological support, helping women to cope with the emotional and social changes that may accompany menopause. By promoting awareness and understanding of menopause, women can be better prepared for the changes it brings and more adept at seeking out and utilizing the support available to them.
In conclusion, empowering women through menopause education is a multifaceted endeavor that involves open communication with healthcare providers, advocacy for personalized care, and the provision of comprehensive resources and support. By addressing these key areas, we can ensure that women are equipped with the knowledge and confidence to navigate the menopausal transition with dignity and autonomy.











