Defining Menopause and Perimenopause
Menopause is a natural biological process that marks the end of a woman’s reproductive years. It is officially diagnosed after a woman has gone without menstruating for 12 consecutive months. The average age for reaching menopause is 51, although it can occur anytime between the ages of 40 and 58. Perimenopause, or the menopausal transition, refers to the period leading up to menopause when the ovaries gradually begin to produce less estrogen. This phase can start in a woman’s mid-30s to mid-50s and typically lasts for four to eight years.
Biological Changes During Menopause
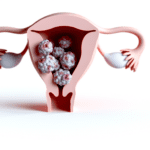
During menopause, the body undergoes significant hormonal changes, primarily characterized by a decrease in estrogen and progesterone production by the ovaries. These changes can lead to a variety of symptoms, including irregular periods, hot flashes, night sweats, mood swings, and vaginal dryness. The decline in estrogen also contributes to long-term health risks such as osteoporosis and changes in cholesterol levels, which can increase the risk of heart disease.
Common Misconceptions About Menopause
There are several misconceptions surrounding menopause that can cause confusion and anxiety. One common myth is that menopause always starts at age 50, but in reality, the timing varies greatly among women. Another misconception is that menopause results in the immediate cessation of menstruation; however, the transition can be gradual with varying menstrual patterns. Additionally, while many believe that menopause leads to a decline in sexual function, many women continue to enjoy satisfying sexual relationships post-menopause. Lastly, it is often thought that menopause can be diagnosed with a single hormone test, but due to fluctuating hormone levels, a diagnosis is more accurately made by evaluating symptoms and menstrual history.
Identifying Symptoms of Menopause
Physical Symptoms and Their Variability
Menopause is a natural biological process that marks the end of menstrual cycles, typically occurring in a woman’s 40s or 50s. The physical symptoms of menopause can be diverse and vary significantly from one individual to another. Irregular periods are often one of the first signs, with cycles that may become longer or shorter, heavier or lighter, and more or less frequent. Eventually, periods will cease altogether.
Other common physical symptoms include vasomotor symptoms such as hot flashes and night sweats, which can cause sudden warmth, flushing, and sweating. Vaginal dryness can lead to discomfort during intercourse, while changes in skin and hair texture, such as increased dryness or thinning, are also prevalent. Women may experience weight gain, particularly around the waist, and a decrease in muscle mass. Joint stiffness and aches are not uncommon, and some women report an increase in facial hair due to hormonal changes.
It’s important to note that the intensity and duration of these symptoms can vary widely. Some women may have mild symptoms that last a short time, while others may experience severe symptoms that significantly impact their quality of life for many years.
Psychological and Emotional Changes
Menopause can also bring about significant psychological and emotional changes. Many women report experiencing mood swings, anxiety, and depression. A lack of motivation, difficulty concentrating, and feelings of tension may also occur. These emotional changes can be exacerbated by sleep disturbances caused by night sweats or other menopausal symptoms.
It’s not uncommon for women to experience a sense of loss or a decline in self-confidence during this time. Memory problems and the phenomenon known as “brain fog” can contribute to feelings of frustration and self-doubt. However, it’s crucial to recognize that these symptoms are normal and often temporary. Engaging in mentally stimulating activities, regular exercise, and seeking support from healthcare professionals and support groups can be beneficial.

From unhappy, dry, and sandpaper to silky, smooth and feeling good. That’s Cleo. Cleo is a 100% natural labial balm to moisture and soothe “your other lips”. Cleo is chemical-free, water-free, pH optimized and helps maintain and restore your delicate labial skin’s natural flora. Ideal for daily use or as needed. Get the most silky, lovable lips ever.
The Importance of Tracking Menstrual Cycles
One practical step women can take to better understand their transition into menopause is to track their menstrual cycles. Noting changes in frequency, duration, and flow can provide valuable insights into whether menopause is approaching. This tracking can also help differentiate between normal perimenopausal patterns and symptoms that may indicate other health issues.
Tracking menstrual cycles can also be helpful when consulting with healthcare professionals. It provides a clear record of changes and can assist in discussions about symptom management and treatment options. Moreover, since pregnancy is still possible during perimenopause, understanding one’s cycle can inform decisions about contraception.
In summary, while menopause is a natural stage of life, its symptoms can significantly impact physical, emotional, and psychological well-being. Being informed about the symptoms and tracking menstrual changes can empower women to seek the support and treatment they need to navigate this transition more comfortably.
Hormonal Fluctuations and Diagnostic Tests
The Role of Hormones in Menopause
Menopause is a natural biological process that marks the end of a woman’s reproductive years. This transition is primarily driven by hormonal fluctuations, particularly the decline in estrogen and progesterone production by the ovaries. As women approach menopause, their menstrual cycles become irregular, a phase known as perimenopause, before ceasing entirely. The hallmark of menopause is the cessation of menstrual periods for 12 consecutive months. During this time, the levels of follicle-stimulating hormone (FSH) typically increase, while estrogen levels decrease. These hormonal changes are responsible for many of the physical and emotional symptoms associated with menopause.
Limitations of Hormone Testing
While hormone levels are central to the changes experienced during menopause, testing these levels to diagnose menopause can be challenging. Hormone levels, particularly estrogen and FSH, can fluctuate significantly during perimenopause, making it difficult to draw definitive conclusions from a single test. For instance, a woman may have elevated FSH levels one day, suggesting menopause, but lower levels the next. Additionally, certain hormone therapies, such as birth control pills, can affect the validity of FSH tests. As a result, hormone testing is not typically used as a standalone diagnostic tool for menopause.
Alternative Diagnostic Approaches
Given the limitations of hormone testing, healthcare professionals often rely on a comprehensive evaluation of a woman’s medical history, menstrual history, and symptoms to diagnose menopause. Common symptoms include changes in menstrual patterns, hot flashes, night sweats, and vaginal dryness. In some cases, blood tests may be conducted to rule out other conditions with similar symptoms, such as thyroid disorders. Over-the-counter urine tests that measure FSH levels are available but are not considered informative due to the same variability seen in blood tests. Ultimately, the diagnosis of menopause is a clinical one, based on the absence of menstrual periods for one year and the presence of menopausal symptoms, rather than on the results of hormone tests alone.

Doubting chemicals in skincare and femcare? Well done! Choose chemical-free products whenever possible.
The Ineffectiveness of Saliva Testing
Challenges with Salivary Hormone Level Tests
Saliva testing for hormone levels has been marketed as a convenient and non-invasive method for assessing hormonal status, particularly during menopause. However, there are significant challenges associated with this type of testing. One of the primary issues is the variability in saliva production among individuals, which can be influenced by factors such as hydration, time of day, and recent food intake. This variability can lead to inconsistent results that may not accurately reflect an individual’s hormonal balance.
Moreover, the presence of enzymes and antibodies in saliva can alter hormone levels, potentially skewing test results. The act of collecting saliva itself can be a source of stress for some individuals, which may influence cortisol levels and other stress-related hormones, further complicating the interpretation of results.
Another challenge is the potential for contamination of the saliva sample, whether from food particles, cosmetics, or blood micro-damage from tooth brushing, which can particularly affect testosterone readings. These factors can introduce significant errors into the testing process, making it difficult to rely on saliva testing as a definitive measure of hormonal status.
Why Saliva Testing Is Not Recommended
Given the challenges outlined above, saliva testing is generally not recommended for accurately diagnosing menopause or for monitoring hormone therapy. The North American Menopause Society and other expert bodies have expressed concerns about the reliability of saliva tests, particularly due to the distortion of hormone levels following the use of exogenous hormones, such as those found in hormone replacement therapies.
Saliva testing often requires individuals to abstain from hormone use for a period before sample collection, which can be impractical and uncomfortable, especially for those relying on hormones for symptom relief. Additionally, saliva tests typically measure only free hormone levels and do not provide information on hormone metabolites, which are crucial for understanding the full picture of hormone metabolism and its implications for health.
Furthermore, saliva testing does not account for the pulsatile nature of hormone secretion, offering only a snapshot of hormone levels at a single point in time. This limitation can lead to misinterpretation of a person’s hormonal status, as hormone levels can fluctuate significantly throughout the day.
In light of these limitations, more reliable diagnostic approaches, such as blood serum and urine testing, are favored. These methods provide a more comprehensive assessment of hormone levels and their metabolites, offering a clearer understanding of a person’s hormonal health during menopause.

Bette 100% All-Natural Relaxing Lavender Body Lotion.
Chemical-Free
Your relaxing night time body moisturizer to leave the day’s stress behind. Decompress and wish your body good night with the calming scent of lavender.
Follicle-Stimulating Hormone (FSH) Testing
Understanding FSH Levels and Menopause Confirmation
Follicle-Stimulating Hormone (FSH) is a key hormone involved in the regulation of the reproductive process. In women, FSH stimulates the growth of ovarian follicles before the release of an egg during ovulation. As a woman approaches menopause, her ovaries gradually cease functioning, leading to a decrease in estrogen production. This hormonal shift causes the body to increase FSH production in an attempt to stimulate the ovaries. A blood level of FSH that is consistently elevated to 30 mIU/mL or higher, coupled with the absence of menstruation for a year, is generally accepted as confirmation of menopause.
The Inconsistency of FSH as a Menopause Indicator
While FSH levels can provide insights, they are not a definitive indicator of menopause due to their variability. During perimenopause, the period leading up to menopause, FSH and estrogen levels can fluctuate significantly. A single elevated FSH reading may not necessarily indicate menopause, as levels can rise and fall throughout the menstrual cycle. Conversely, a low FSH level does not rule out perimenopause, even in the presence of symptoms such as hot flashes and menstrual irregularities. Therefore, relying solely on an FSH test for menopause confirmation can be misleading.
The Impact of Hormone Therapies on FSH Test Validity
The use of certain hormone therapies, such as birth control pills, can affect the validity of an FSH test. These treatments can artificially alter hormone levels, masking the natural rise in FSH associated with menopause. Consequently, healthcare professionals may advise discontinuing hormone therapies for a period before testing FSH levels to obtain an accurate reading. Additionally, over-the-counter urine tests that measure FSH levels are not recommended due to their high cost and limited informative value, as they are subject to the same fluctuations and inaccuracies as blood tests.
In summary, while FSH testing can be a component of the menopause diagnosis process, it should not be used in isolation. A comprehensive evaluation that includes a review of medical history, menstrual history, and symptoms is essential for an accurate diagnosis. Healthcare providers may also consider other tests and factors before concluding a woman’s menopausal status.
Navigating Perimenopause with Professional Guidance
The Role of Medical History in Diagnosing Perimenopause
Understanding the nuances of perimenopause often begins with a comprehensive review of a woman’s medical history. A healthcare professional will consider several factors, including age, menstrual history, and the presence of symptoms commonly associated with hormonal changes. This historical data is crucial because hormone levels fluctuate significantly during perimenopause, making it challenging to rely solely on laboratory tests for a diagnosis.
During a medical consultation, the healthcare provider will inquire about the regularity and characteristics of menstrual cycles, the onset of symptoms such as hot flashes or sleep disturbances, and any changes in mood or sexual function. This information helps to paint a clearer picture of whether a woman is entering the perimenopausal phase. It’s also an opportunity to rule out other conditions that may mimic perimenopausal symptoms, such as thyroid disorders.

If you wonder, if this discomfort and the dryness down there will be there forever….
Try Mae. Mae is gives you back comfort, control, re-assurance, and re-connecting.
Mae is more than just a vaginal moisturizer; it’s your ally for intimate natural health, rediscovering joy, cultivating comfort, and even igniting sparks of intimacy and rekindled romance. Mae is your companion in rejoicing in your femininity at every stage of life. Learn more…
When to Consult a Healthcare Professional
It’s advisable to seek professional guidance when you notice changes that may signal the onset of perimenopause. These changes can include but are not limited to, irregular menstrual cycles, hot flashes, night sweats, vaginal dryness, and mood swings. Consulting a healthcare professional becomes even more critical if these symptoms disrupt daily life or cause significant discomfort.
Additionally, women who experience symptoms of perimenopause at a relatively young age, those with a history of certain cancers, or individuals with risk factors for osteoporosis should discuss these concerns with their healthcare provider. Early intervention and guidance can help manage symptoms effectively and address any potential health risks associated with hormonal changes.
The Comprehensive Medical Examination Process
The process of diagnosing perimenopause typically involves a thorough medical examination. This examination may include:
- Physical Assessment: A general physical exam to check for any physical signs of hormonal changes.
- Review of Symptoms: A detailed discussion of symptoms, their severity, and their impact on quality of life.
- Menstrual History: An analysis of menstrual cycle patterns and any recent changes.
- Family Medical History: Gathering information about the menopausal experiences of close relatives, which can sometimes offer clues about one’s own transition.
- Possible Laboratory Tests: While not always necessary, certain tests may be ordered to rule out other conditions or to check overall health. For example, thyroid function tests are sometimes conducted as thyroid issues can mimic perimenopausal symptoms.
It’s important to note that while hormone tests are not typically the primary tool for diagnosing perimenopause, they may be used in specific circumstances, such as evaluating fertility concerns or when periods cease at an early age.
Ultimately, the goal of the medical examination is to provide a personalized assessment that takes into account all aspects of a woman’s health and well-being during this transitional phase. By partnering with a healthcare professional, women can navigate perimenopause with informed decisions about their health and treatment options.
Future Directions and Ongoing Research
Menopause Prediction and Confirmation
Despite advancements in understanding menopause, predicting and confirming its onset remains a challenge. The variability in age and symptoms among individuals and across ethnicities complicates the creation of a universal model for menopause prediction. Current diagnostic methods rely heavily on self-reported symptoms and menstrual history, which can be subjective and influenced by cultural and personal perceptions. Moreover, the hormonal changes that signify menopause can be erratic, making it difficult to pinpoint the transition with precision. The lack of reliable biomarkers that can consistently indicate the onset of menopause further hinders the development of predictive tools. As a result, many women are left uncertain about their menopausal status, leading to potential delays in receiving appropriate care and support.
Emerging Research and Potential Breakthroughs
Research into menopause is rapidly evolving, with new studies focusing on genetic, molecular, and environmental factors that contribute to the menopausal transition. Scientists are exploring the role of genetic markers and polymorphisms that may predict the timing of menopause, potentially leading to personalized risk assessments. Advances in omics technologies, such as genomics, proteomics, and metabolomics, are being leveraged to uncover novel biomarkers that could offer more definitive indicators of menopause. Additionally, there is growing interest in the impact of lifestyle factors, such as diet and exercise, on menopausal symptoms and timing. These research avenues hold promise for more accurate predictions of menopause and tailored interventions that could mitigate symptoms and improve quality of life for women undergoing this transition.
Staying Informed Through Reliable Sources
Given the complexity of menopause and the ongoing nature of research, it is crucial for women to access reliable and up-to-date information. Healthcare professionals should be a primary source of knowledge, providing evidence-based guidance and support. Women are also encouraged to seek information from reputable organizations and research institutions that specialize in menopausal health. Staying informed about the latest findings can empower women to make educated decisions about their health and to participate actively in discussions about potential treatments and lifestyle modifications. As the scientific community continues to unravel the intricacies of menopause, disseminating this knowledge will be key to improving the menopausal experience for women worldwide.
By the way, something for you, a little gift!!!
I am just in the middle of publishing my book. It’s about How women can balance their hormones. One part is about food and diet, of course.
Follow this link and enter your email.
I will send you this part of the book for free once the book is published. It has many concrete, practical tips and recipes and will help you feel better during menopause or times of Big hormonal fluctuations.
Annette, Damiva Lead for Health & Wellness