Understanding Hot Flashes
Hot flashes are a common symptom of menopause characterized by a sudden feeling of warmth that spreads over the body, often accompanied by a flushed appearance and sweating. They are considered a vasomotor symptom due to their association with changes in blood vessel dilation. While typically associated with the menopausal transition, hot flashes can also occur due to other medical conditions or as side effects of certain medications.
Symptoms and Sensations
The experience of a hot flash can vary from person to person but generally includes a sensation of heat, particularly in the upper body, face, and neck. This can lead to redness, sweating, and sometimes palpitations. Following the heat, individuals may feel chilled or experience a cold sweat. The intensity, frequency, and duration of these symptoms can differ significantly among individuals, affecting their quality of life to varying degrees.
Duration and Severity Variations
Hot flashes can last from a few seconds to several minutes and may occur a few times a week or several times a day. The severity ranges from mild and tolerable to severe and disruptive. The average duration of hot flashes is typically between 6 months to 2 years, but some individuals may experience them for a decade or longer, and in rare cases, they may persist indefinitely.
Underlying Mechanisms
The exact cause of hot flashes is not fully understood, but they are believed to be related to changes in the hypothalamus, the part of the brain responsible for regulating body temperature. Fluctuations in estrogen levels during menopause are thought to affect the hypothalamus’s ability to accurately sense body temperature, leading to the dilation of blood vessels and subsequent heat sensation. This complex process reflects the body’s attempt to cool down, despite not actually overheating.

Bette 100% All-Natural Relaxing Lavender Body Lotion.
Chemical-Free
Your relaxing night time body moisturizer to leave the day’s stress behind. Decompress and wish your body good night with the calming scent of lavender.
Onset and Longevity of Hot Flashes
Typical Age of Onset
Hot flashes are a hallmark symptom of menopause, typically beginning in a person’s late 40s to early 50s. However, the onset can vary widely, with some experiencing these symptoms earlier or later than this average range. The onset of hot flashes is closely tied to the hormonal changes that occur during the menopausal transition, a period also known as perimenopause. This phase can precede the cessation of menstrual periods by several years, during which time many may start to experience the characteristic sudden sensations of heat.
Post-Menopausal Persistence
Contrary to the common belief that hot flashes cease shortly after menopause, they can persist well into the post-menopausal years. The duration of hot flashes varies significantly among individuals. While some may experience relief within 6 to 24 months, others endure symptoms for much longer—up to 7 to 11 years, according to the Study of Women’s Health Across the Nation (SWAN). In certain cases, hot flashes may continue indefinitely, with occurrences even reported in individuals in their 70s and beyond. The persistence of hot flashes post-menopause can affect quality of life and sleep patterns, often necessitating medical consultation and intervention.
Factors Influencing Duration
The duration and severity of hot flashes are influenced by several factors:
- Timing of Onset: Women who experience hot flashes before the end of their menstrual periods tend to have them for a longer duration—about nine to ten years on average. In contrast, those whose hot flashes start after their last menstrual period typically experience them for a shorter time, around three and a half years.
- Lifestyle Factors: Smoking, body weight, and stress levels have been associated with a longer duration of hot flashes. Smokers or those with obesity may find that their symptoms persist for a more extended period.
- Ethnicity: Ethnic background also plays a role, with African American women reporting the longest duration of hot flashes, while Japanese and Chinese women tend to experience them for a shorter time.
- Health Status: Underlying health conditions, such as thyroid disorders or mental health issues like depression and anxiety, can also affect the longevity of hot flashes.
Understanding these factors can help individuals and healthcare providers develop personalized strategies for managing symptoms effectively. It is essential for those experiencing hot flashes to discuss their symptoms with a healthcare provider, who can offer guidance on both medical treatments and lifestyle adjustments to alleviate discomfort.
Identifying and Managing Triggers
Common Triggers
Hot flashes are a hallmark symptom of menopause, often described as a sudden sensation of heat that spreads through the body. Understanding what triggers these episodes can be key to managing their occurrence and severity. Common triggers include:
- Environmental temperature: Being in a hot environment or experiencing weather changes can provoke a hot flash.
- Dietary stimulants: Consuming caffeine, alcohol, or spicy foods has been linked to the onset of hot flashes.
- Nicotine: Smoking or exposure to cigarette smoke can trigger hot flashes, highlighting another benefit of smoking cessation.
- Stress: Emotional stress is a well-known trigger that can lead to a hot flash episode.
Dietary Considerations
What you eat and drink plays a significant role in managing hot flashes. To minimize episodes, consider the following dietary adjustments:
- Avoid or limit caffeine, alcohol, and spicy foods, which are known to trigger hot flashes.
- Incorporate foods rich in phytoestrogens, such as soybeans, chickpeas, and lentils, which may have a mild estrogen-like effect on the body.
- Stay hydrated with cool beverages, particularly water, to help regulate body temperature.
Do you know the three main ways that your body gets in touch with harmful chemicals with everyday products? Knowledge is Power!
The Ultimate Detox Guide will tell you how to lower your exposure to harmful chemicals!

Environmental and Lifestyle Factors
Your surroundings and lifestyle choices can significantly influence the frequency and intensity of hot flashes. To create a more comfortable environment:
- Dress in layers that can be easily removed during a hot flash.
- Keep your living and workspaces cool with fans or air conditioning.
- Practice regular exercise, which can help manage weight and reduce stress, potentially decreasing the frequency of hot flashes.
Stress and Emotional Well-being
Stress is a common trigger for hot flashes, and managing stress levels can help reduce their occurrence. Techniques to enhance emotional well-being include:
- Engaging in relaxation practices such as yoga, meditation, or deep-breathing exercises.
- Seeking support from friends, family, or support groups to share experiences and coping strategies.
- Considering cognitive-behavioral therapy or counseling to develop stress management skills.
By identifying personal triggers and implementing lifestyle and dietary changes, individuals can effectively manage hot flashes and improve their quality of life during menopause.
Medical Treatments for Hot Flashes
Hormone Replacement Therapy (HRT)
Hormone Replacement Therapy (HRT) is often considered the most effective treatment for hot flashes and other menopausal symptoms. HRT works by replenishing the body with estrogen and, in women with a uterus, progesterone to counteract the hormonal fluctuations that contribute to hot flashes. There are various forms of HRT, including pills, patches, gels, and creams. The specific regimen a healthcare provider prescribes will depend on the individual’s health history and the severity of their symptoms. While HRT can be highly effective, it is not suitable for everyone, particularly those with a history of certain cancers, blood clotting disorders, or severe cardiovascular disease.
Non-Hormonal Prescription Medications
For individuals who cannot use HRT, non-hormonal prescription medications offer an alternative. These include certain antidepressants like selective serotonin reuptake inhibitors (SSRIs), which have been found to reduce the frequency and severity of hot flashes. Medications such as venlafaxine, desvenlafaxine, fluoxetine, paroxetine (the only FDA-approved SSRI for hot flashes), and escitalopram are commonly prescribed. Other non-hormonal options include gabapentin, which is effective for hot flashes that disrupt sleep, and clonidine, which can provide relief for some individuals. The recent FDA approval of Veozah, a neurokinin 3 (NK3) receptor antagonist, provides a new avenue for those who do not respond to other treatments.
Evaluating Effectiveness and Side Effects
When considering medical treatments for hot flashes, it is crucial to evaluate the effectiveness and potential side effects of each option. Hormone therapy may offer significant relief but comes with risks such as an increased chance of blood clots, stroke, and certain cancers. Non-hormonal medications can also have side effects, ranging from nausea and headaches to changes in blood pressure and mood. It is important to monitor the body’s response to a new medication and report any adverse effects to a healthcare provider promptly.
Consulting Healthcare Providers
Before starting any treatment for hot flashes, it is essential to consult with a healthcare provider. A provider can offer a personalized assessment based on medical history, current health status, and other medications being taken. They can also provide guidance on the risks and benefits of each treatment option, helping to make an informed decision. For those seeking a specialist in menopause management, resources such as The North American Menopause Society offer directories to find qualified professionals.
Ultimately, the choice of treatment should be made in collaboration with a healthcare provider, considering all available information and personal health needs. With the right approach, it is possible to manage hot flashes effectively and improve overall quality of life during menopause.
Feeling You Have a Right to Safe Beauty & Fem Care?
If so, it may be time for a change. It starts with knowledge. We have a few suggestions in our new guides.
Alternative and Over-the-Counter Remedies
Herbal Supplements and Efficacy
Many women seek out herbal supplements as a natural approach to alleviate hot flashes. Among the most popular are black cohosh, red clover, evening primrose oil, and soy. While some small-scale studies have suggested potential benefits, the overall evidence for their effectiveness is mixed. For instance, black cohosh has been studied for its possible benefits in reducing menopausal symptoms, but results are inconclusive and some studies show no improvement over placebos. Similarly, soy contains phytoestrogens, which are thought to have weak estrogen-like effects, but clinical studies have largely shown that they are not effective for the treatment of hot flashes.
Safety and Risks of Botanicals
When considering botanicals, safety is a significant concern. For example, black cohosh should be used with caution as it may cause liver toxicity and should not be used for more than six months. Red clover may increase the risk of bleeding, especially in women taking blood thinners. Evening primrose oil may interact with psychiatric medications and blood thinners. It is crucial to note that the U.S. Food and Drug Administration (FDA) does not regulate herbal supplements for quality and purity as it does for prescription medications, which means there can be considerable variability in the content and concentration of active ingredients.
Vitamins and Non-Prescription Options
Vitamin E has been explored as a potential remedy for hot flashes, with one study indicating a slight reduction in symptoms. However, the benefits were modest, and there are concerns about long-term use, including an increased risk of heart failure and other cardiovascular events. It is essential to weigh these risks against the potential for only marginal relief of hot flashes.
Assessing Legitimacy and Claims
When evaluating over-the-counter products, it’s important to critically assess their legitimacy and claims. Be wary of products that promise a “cure” or make exaggerated claims without scientific backing. Always check for a complete list of ingredients and be cautious of “secret formulas.” Testimonials can be misleading as they often represent only the positive outcomes and may be incentivized. The most reliable approach is to consult with a healthcare provider before starting any new treatment for hot flashes. They can help determine whether a product is safe based on your medical history, current medications, and overall health condition.
In conclusion, while alternative and over-the-counter remedies may offer some hope for relief from hot flashes, it is vital to approach them with caution. The efficacy of herbal supplements is not consistently supported by scientific evidence, and safety concerns must be taken seriously. Vitamins and other non-prescription options may have some benefits, but they also come with risks. Always consult with a healthcare provider to ensure that any treatment chosen is safe and appropriate for your individual needs.

Lifestyle Adjustments to Alleviate Hot Flashes
Diet and Weight Management
Maintaining a healthy diet and weight can be a powerful strategy in managing hot flashes. Obesity has been linked to more frequent and severe hot flashes. A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help regulate the body’s temperature and reduce the occurrence of hot flashes. Incorporating foods with plant estrogens, such as soybeans, chickpeas, lentils, and flaxseed, may offer some relief due to their weak estrogen-like effects. However, it’s important to focus on natural food sources rather than supplements, as the latter can have inconsistent doses and questionable efficacy.
Exercise and Physical Activity
Regular physical activity is beneficial for overall health and can help reduce the severity of hot flashes. Exercise can improve mood, aid in weight management, and promote better sleep, all of which can mitigate menopausal symptoms. Aim for at least 30 minutes of moderate exercise most days of the week, but be mindful of the environment to avoid overheating, which can trigger hot flashes. Activities such as swimming, walking in cool weather, or indoor aerobics in a well-ventilated room are excellent choices.
Environmental and Habitual Changes
Small adjustments in your daily environment can make a significant difference in managing hot flashes. Dress in layers that can be easily removed during a hot flash, and use a fan or air conditioning to maintain a cool environment at home and work. At night, lower the bedroom temperature and consider using moisture-wicking bedding to combat night sweats. Additionally, practicing relaxation techniques such as deep breathing, yoga, or meditation can help reduce stress and the frequency of hot flashes.
Tobacco Use and Its Impact
Smoking and tobacco use have been associated with an increase in the frequency and intensity of hot flashes. Nicotine affects the body’s ability to regulate temperature, and smoking can exacerbate menopausal symptoms. Quitting smoking is not only beneficial for reducing hot flashes but also improves overall health and reduces the risk of numerous diseases. For those struggling to quit, seeking support from healthcare providers or smoking cessation programs can provide the necessary tools and resources for success.
By implementing these lifestyle adjustments, individuals can gain a sense of control over their hot flashes and improve their quality of life during the menopausal transition
By the way, something for you, a little gift!!!
I am just in the middle of publishing my book. It’s about How women can balance their hormones. One part is about food and diet, of course.
Follow this link and enter your email.
I will send you this part of the book for free once the book is published. It has many concrete, practical tips and recipes and will help you feel better during menopause or times of Big hormonal fluctuations.
Annette, Damiva Lead for Health & Wellness

Coping with Menopause-Related Emotional Changes
Mood Swings, Depression, and Anxiety
Menopause can be a rollercoaster of emotions. Mood swings may have you feeling joyful one moment and tearful the next, while depression and anxiety can set in due to hormonal fluctuations and the stress of physical changes. It’s important to recognize that these emotional responses are common and there are ways to manage them. If feelings of sadness or worry become overwhelming, it’s crucial to seek help from a healthcare provider.
Self-Calming Techniques and Hobbies
Engaging in self-calming activities and hobbies can be a powerful way to manage menopause-related emotional changes. Techniques such as yoga, meditation, and deep breathing exercises can help to reduce stress and promote relaxation. Finding a creative outlet, like painting, writing, or gardening, can also provide a sense of achievement and joy.
Social Support and Community Engagement
Building a strong support network is essential during menopause. Staying connected with family and friends provides emotional support and can help you navigate this transition more smoothly. Community engagement, whether through volunteer work, clubs, or support groups, can also offer a sense of belonging and purpose.
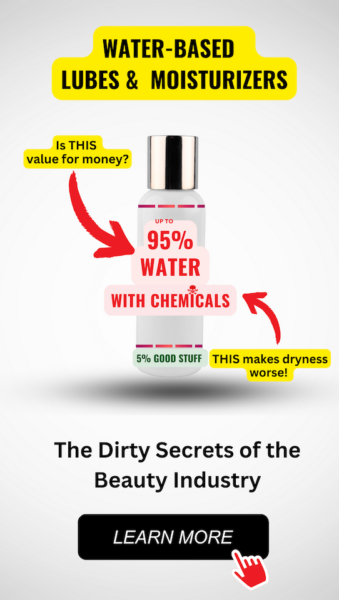
Addressing Painful Intercourse
Painful intercourse is a common issue during menopause, often due to vaginal dryness. Using water-free, chemical-free lubricants or moisturizers can alleviate discomfort. It’s also important to communicate openly with your partner about your needs and to explore different forms of intimacy that may be more comfortable. If pain persists, consult a healthcare provider for additional treatment options.

From unhappy, dry, and sandpaper to silky, smooth and feeling good. That’s Cleo. Cleo is a 100% natural labial balm to moisture and soothe “your other lips”. Cleo is chemical-free, water-free, pH optimized and helps maintain and restore your delicate labial skin’s natural flora. Ideal for daily use or as needed. Get the most silky, lovable lips ever.
Remember, menopause is a natural phase of life, and with the right strategies, you can maintain your emotional well-being and continue to enjoy a fulfilling life.