Understanding Perimenopause and Anxiety
Perimenopause marks the transition period leading up to menopause, the point when a woman’s menstrual cycles permanently cease. This phase can span several years, during which women experience fluctuations in their menstrual cycle and a variety of physical and emotional symptoms. It typically begins in a woman’s 40s but can start earlier. The hallmark of perimenopause is irregular menstrual periods that eventually lead to their end, signaling the onset of menopause.
The Link Between Hormonal Changes and Anxiety
Hormonal changes during perimenopause are significant, as the body begins to produce less estrogen and progesterone. These fluctuations can have a profound impact on mood and are closely linked to increased feelings of anxiety. For women with brains sensitive to these hormonal shifts, anxiety can become a prominent feature of their perimenopausal experience. Additionally, physical symptoms such as hot flashes and sleep disturbances can exacerbate anxiety levels.
Symptoms of Perimenopausal Anxiety
Perimenopausal anxiety can manifest in various ways, often resembling general anxiety symptoms. Women may experience:
- Nervousness, irritability, or restlessness
- Difficulty relaxing and an increase in worry
- Challenges with concentration and memory
- Muscle tension and sweating
- Sleep disturbances, including trouble falling or staying asleep
In some cases, perimenopausal anxiety can lead to panic attacks, characterized by dizziness, chest pain, rapid heartbeat, and intense fear.

Bette 100% All-Natural Relaxing Lavender Body Lotion.
Chemical-Free
Your relaxing night time body moisturizer to leave the day’s stress behind. Decompress and wish your body good night with the calming scent of lavender.
The Impact of Life Transitions on Anxiety
Perimenopause coincides with a period in life often filled with significant transitions. Women may be dealing with the challenges of raising teenagers, experiencing empty nest syndrome, facing career changes, or navigating the complexities of “gray divorce.” These life events can contribute to heightened anxiety, making it difficult to pinpoint whether symptoms are solely due to hormonal changes or the stress of these concurrent life changes. Understanding the multifaceted nature of anxiety during this time is crucial for effective management and treatment.
The Biological Basis of Perimenopause-Related Anxiety
Estrogen Fluctuations and Brain Function
The perimenopausal period is marked by significant fluctuations in estrogen levels, which can have profound effects on brain function and mood regulation. Estrogen interacts with neurotransmitter systems, including serotonin and norepinephrine, which are implicated in the regulation of mood and anxiety. During perimenopause, the erratic changes in estrogen can disrupt these neurotransmitter systems, leading to increased vulnerability to anxiety. Additionally, estrogen has neuroprotective properties, and its decline may contribute to changes in brain structures associated with emotion regulation, such as the hippocampus and amygdala, further exacerbating anxiety symptoms.
Physical Symptoms Contributing to Anxiety
Perimenopause is often accompanied by a range of physical symptoms that can contribute to the development or exacerbation of anxiety. These include hot flashes, sleep disturbances, fatigue, and palpitations. The unpredictability and discomfort of these symptoms can lead to heightened anxiety and fear of their occurrence, creating a feedback loop that perpetuates both the physical and psychological symptoms of perimenopause.
Anxiety Sensitivity and Perimenopause
Anxiety sensitivity, or the fear of anxiety-related sensations, may be heightened during perimenopause. As women experience various physical changes, those with high anxiety sensitivity may misinterpret these normal perimenopausal symptoms as signs of serious medical conditions, leading to increased anxiety and worry. This heightened sensitivity to bodily sensations can make perimenopausal women more susceptible to panic attacks and other anxiety-related disorders.
Diagnosing Perimenopausal Anxiety
Screening and Assessment Tools
Identifying anxiety during perimenopause can be challenging due to the overlap of symptoms with other mood disorders and life stressors. However, healthcare professionals have developed validated screening tests to better understand and identify anxiety symptoms. One such tool is the Generalized Anxiety Disorder 7-item (GAD-7) scale, which assesses the frequency of anxiety-related symptoms over the past two weeks. This tool helps to quantify the severity of anxiety and is a useful starting point for further evaluation.
Professional Diagnosis of Anxiety Disorders
Following initial screening, a thorough assessment by a healthcare professional is crucial for an accurate diagnosis. This process involves a detailed discussion about the patient’s symptoms, their onset, and factors that may alleviate or exacerbate them. If anxiety symptoms are significantly impacting daily functioning, a diagnosis of an anxiety disorder may be considered. It is important to note that anxiety can manifest differently in perimenopausal women, sometimes presenting with physical symptoms such as heart palpitations or hot flashes, which can complicate the diagnostic process.
Differentiating Between Anxiety and Other Mood Disorders
Perimenopausal anxiety must be distinguished from other mood disorders, such as depression, which often co-occurs during this life stage. While both conditions can share symptoms like irritability and sleep disturbances, anxiety is typically characterized by persistent worry and tension. Additionally, the timing of symptom onset can provide clues; for instance, perimenopausal mood instability may present with symptoms that do not follow a menstrual cycle pattern, unlike premenstrual syndrome (PMS).
Moreover, the assessment should consider the broader context of the patient’s life, including stressors such as career changes, relationship issues, or caregiving responsibilities. These factors can contribute to or exacerbate anxiety symptoms. A comprehensive evaluation will help healthcare providers develop an individualized treatment plan that addresses both the psychological and physiological aspects of perimenopausal anxiety.
By the way, something for you, a little gift!!!
I am just in the middle of publishing my book. It’s about How women can balance their hormones. One part is about food and diet, of course.
Follow this link and enter your email.
I will send you this part of the book for free once the book is published. It has many concrete, practical tips and recipes and will help you feel better during menopause or times of Big hormonal fluctuations.
Annette, Damiva Lead for Health & Wellness

Treatment and Management Strategies
Lifestyle Modifications for Anxiety Reduction
Adopting certain lifestyle changes can significantly reduce anxiety symptoms during perimenopause. Good sleep hygiene is crucial, as poor sleep can exacerbate anxiety. Avoiding stimulants like caffeine and alcohol, especially later in the day, can improve sleep quality. Stress-reduction techniques such as meditation, yoga, or deep-breathing exercises can also promote relaxation and alleviate anxiety. Additionally, maintaining a balanced diet and staying socially active can have positive effects on mood and overall well-being.
Hormone Replacement Therapy (HRT) and Its Role
Hormone Replacement Therapy (HRT) may not be the first line of treatment for anxiety, but it can alleviate some perimenopausal symptoms that contribute to anxiety, such as vasomotor symptoms (VMS) and sleep disturbances. HRT involves the administration of estrogen or a combination of estrogen and progestin to balance hormone levels. It’s important to discuss the potential benefits and risks of HRT with a healthcare provider, as it may not be suitable for everyone.
Exercise as a Therapeutic Intervention
Regular aerobic exercise has been shown to improve anxiety in perimenopausal individuals. Activities that raise the heart rate, such as dancing, brisk walking, or jogging, can be particularly beneficial. Exercise not only helps in reducing anxiety but also improves sleep, strengthens bones, and enhances cardiovascular health. Whether done individually or in a group, the key is consistency and finding an enjoyable form of exercise.
Medications and Alternative Treatments
Various medications can be prescribed to manage anxiety during perimenopause. Antidepressants, especially selective serotonin reuptake inhibitors (SSRIs), can be effective in treating both anxiety and depressive symptoms. Other medications like gabapentin and fezolinetant may also be considered for their off-label use in reducing hot flashes and associated anxiety. For those interested in alternative treatments, phytoestrogens from foods or supplements and black cohosh have been explored, but their efficacy and safety remain uncertain. It is essential to consult with a healthcare provider before starting any new medication or supplement.
Ultimately, the management of perimenopausal anxiety is multifaceted, involving a combination of lifestyle adjustments, possible hormone therapy, exercise, and medication. Each individual’s treatment plan should be tailored to their specific symptoms, health history, and personal preferences, with regular follow-ups to assess efficacy and make necessary adjustments.
Do you know the three main ways that your body gets in touch with harmful chemicals with everyday products? Knowledge is Power!
The Ultimate Detox Guide will tell you how to lower your exposure to harmful chemicals!

Navigating the Duration and Uncertainties of Perimenopause
The Variable Timeline of Perimenopause
The journey through perimenopause is as unique as the individual experiencing it. Unlike the predictable ticking of a clock, the timeline of perimenopause varies widely among women. Typically beginning in a woman’s 40s, this transitional phase can span anywhere from a few short years to over a decade. During this time, the body undergoes a symphony of hormonal fluctuations, leading to an array of symptoms that can ebb and flow in intensity. Understanding that perimenopause is not a one-size-fits-all process is crucial for managing expectations and planning for the road ahead.
Managing Panic Disorders and Sleep Disturbances
Among the challenges of perimenopause, panic disorders and sleep disturbances stand out for their impact on quality of life. The hormonal roller coaster can exacerbate anxiety, leading to increased instances of panic attacks. To navigate these turbulent waters, a combination of lifestyle modifications, such as mindfulness and relaxation techniques, can be paired with professional support when needed. Sleep disturbances, often manifesting as insomnia or disrupted sleep patterns, can be mitigated by establishing a regular sleep routine, creating a restful environment, and considering medical interventions if necessary.
Long-term Health Considerations
As perimenopause paves the way to postmenopause, it’s essential to consider the long-term health implications. The decline in estrogen levels associated with perimenopause can affect bone density, heart health, and more. Proactive measures, including a balanced diet rich in calcium and vitamin D, regular weight-bearing exercise, and medical screenings, can help safeguard against conditions like osteoporosis and cardiovascular disease. By staying vigilant and informed, women can take charge of their health during perimenopause and beyond.
Ultimately, navigating the duration and uncertainties of perimenopause requires patience, self-care, and a willingness to seek support. With a proactive approach and personalized strategies, women can transition through this natural life stage with confidence and grace.
Support Systems and Coping Mechanisms
The Importance of Social Support
During the perimenopausal transition, the importance of social support cannot be overstated. A robust network of friends, family, and peers can provide emotional sustenance, practical advice, and a sense of community that helps mitigate the feelings of isolation and anxiety that often accompany this stage of life. Studies have shown that women with strong social ties experience fewer and less severe symptoms of anxiety during perimenopause. Social support can take many forms, from regular meet-ups with friends to online forums where women share their experiences and coping strategies. The act of sharing and feeling understood itself can be therapeutic, helping to normalize the wide array of emotions and physical changes that occur during this time.
Professional Guidance and Counseling
For many women, professional guidance and counseling are invaluable resources in managing perimenopausal anxiety. Mental health professionals can offer a range of therapeutic approaches, including cognitive behavioral therapy (CBT), which has been shown to be effective in treating anxiety disorders. Counseling provides a safe space to explore feelings, develop coping strategies, and address any underlying issues that may be contributing to anxiety. In some cases, healthcare providers may also recommend group therapy, which combines professional guidance with the benefits of social support, allowing women to learn from others facing similar challenges.
Self-Care and Mindfulness Practices
Self-care is a critical component of managing perimenopausal anxiety. This includes adequate sleep, a balanced diet, and regular physical activity, which can all have a positive impact on mood and anxiety levels. Mindfulness practices, such as meditation, deep breathing exercises, and yoga, can also be particularly beneficial. These practices help women develop a greater awareness of their thoughts and feelings, reduce stress, and promote a sense of calm. By incorporating mindfulness into daily routines, women can cultivate a more centered and peaceful state of mind, better equipping them to handle the ups and downs of perimenopause.
Ultimately, the combination of social support, professional help, and self-care creates a comprehensive approach to managing perimenopausal anxiety. Each element plays a vital role in supporting women through this transition, helping them to maintain their quality of life and well-being.
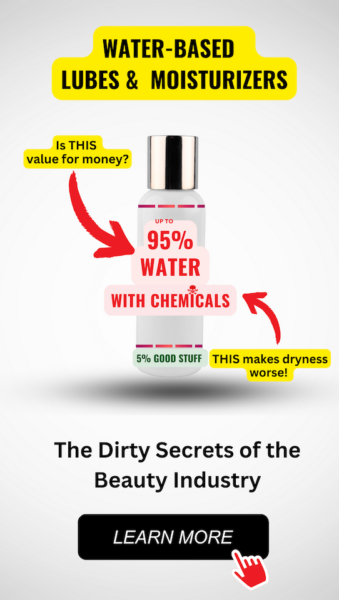
Feeling You Have a Right to Safe Beauty & Fem Care?
If so, it may be time for a change. It starts with knowledge. We have a few suggestions in our new guides.
Broader Health Concerns During Perimenopause
Depression and Its Correlation with Anxiety
Depression is a common mental health issue that can significantly impact the quality of life for perimenopausal women. The hormonal fluctuations that characterize perimenopause can contribute to mood swings and an increased risk of depression. Studies have shown that the risk of developing depression may be higher during perimenopause, even for women without a history of the condition. The link between depression and anxiety is well-established, with many individuals experiencing both concurrently. Anxiety during perimenopause can exacerbate depressive symptoms, creating a challenging cycle of mental health concerns. It is essential for healthcare providers to screen for both depression and anxiety during perimenopause to ensure appropriate treatment and support.
Eating Disorders and Body Image Issues
Body image issues may become more pronounced during perimenopause, as women experience changes in weight, body shape, and skin elasticity. These physical changes can trigger or worsen pre-existing eating disorders or lead to the development of new disordered eating patterns. Healthcare professionals should be vigilant in monitoring signs of eating disorders in perimenopausal patients, as these conditions can have severe health implications and may be less commonly diagnosed in this demographic compared to younger individuals.
Alcohol Consumption and Its Effects
Alcohol consumption can have various effects on perimenopausal women, potentially exacerbating symptoms such as hot flashes and disrupting sleep patterns. Additionally, alcohol can interact with medications commonly prescribed during perimenopause, including antidepressants and hormone replacement therapy (HRT), leading to adverse effects. It is crucial for women to be aware of the risks associated with alcohol use during this transitional period and for healthcare providers to discuss alcohol consumption as part of a comprehensive perimenopausal health assessment.