Defining Osteoporosis and Its Prevalence
Osteoporosis, often described as a “silent disease,” is a condition characterized by weakened bones and an increased risk of fractures. The World Health Organization (WHO) defines osteoporosis based on bone mineral density (BMD) levels measured by dual-energy X-ray absorptiometry (DXA). A T-score of -2.5 or lower indicates osteoporosis. This condition is prevalent, particularly among postmenopausal women, with statistics showing that approximately half of women over the age of 50 will experience an osteoporosis-related fracture in their lifetime.
The Connection Between Menopause and Bone Health
Menopause, which typically occurs between the ages of 45 and 55, marks the end of menstrual cycles and is accompanied by a decline in reproductive hormones, especially estrogen. This hormonal shift is directly linked to a decrease in bone density, accelerating the risk of developing osteoporosis. Postmenopausal women can lose up to 10% of their bone mass in the first five years following menopause, making the connection between menopause and bone health a critical area of concern.
Estrogen’s Role in Bone Density
Estrogen plays a vital role in maintaining bone density by regulating the bone remodeling process, which involves the resorption of old bone and the formation of new bone. During menopause, the drop in estrogen levels disrupts this balance, leading to increased bone resorption without adequate bone formation, resulting in a net loss of bone mass and density.
Risk Factors Beyond Menopause
While menopause is a significant risk factor for osteoporosis, other elements can contribute to bone density loss. These include a sedentary lifestyle, poor nutrition, excessive alcohol consumption, smoking, and the use of certain medications. Genetic factors also play a role, with family history being a strong predictor of osteoporosis risk.
Ethnicity and Osteoporosis Risk
Ethnicity is another factor that influences the risk of developing osteoporosis. Studies have shown that Caucasian and Asian women are at a higher risk compared to African American women. Additionally, the prevalence and age of onset of osteoporotic fractures can vary significantly across different ethnic groups, with some evidence suggesting earlier onset in certain populations.
In conclusion, understanding the interplay between menopause and osteoporosis is essential for the prevention and management of bone health in postmenopausal women. Recognizing the role of estrogen, alongside other risk factors, can help in developing targeted strategies to maintain bone density and reduce the risk of fractures.
Identifying and Managing Risk Factors
Lifestyle Choices and Bone Health
The lifestyle choices we make can have a significant impact on our bone health. Regular physical activity, particularly weight-bearing and muscle-strengthening exercises, is crucial for maintaining bone density. Aim for 30 to 60 minutes of exercise most days of the week. Activities such as walking, jogging, dancing, and resistance training can help slow bone loss and improve overall fitness. Additionally, avoiding smoking and limiting alcohol consumption are important, as these habits can accelerate bone loss and increase the risk of fractures.
Genetic Predisposition and Family History
Genetics play a role in bone health, with a family history of osteoporosis or fractures indicating a higher risk. While we cannot change our genetic makeup, being aware of family history can prompt earlier screening and proactive management. Women, particularly those of Caucasian or Asian descent, are at a higher risk, and small, thin-boned individuals are more susceptible to bone loss.
The Impact of Diet on Bone Density
Diet is a modifiable risk factor that has a direct effect on bone health. A diet rich in calcium and vitamin D is essential for maintaining strong bones. Aim for a daily intake of 1,000–1,500 mg of calcium and 600–800 IU of vitamin D. Foods such as dairy products, leafy greens, and fortified foods contribute to calcium intake, while vitamin D can be synthesized through sun exposure and is also found in fatty fish and fortified foods. For those with dietary restrictions or deficiencies, supplements may be necessary.
Medication and Substance Use
Certain medications can negatively affect bone density, including long-term use of corticosteroids and some anticonvulsants. It’s important to discuss the potential bone-related side effects of any medication with a healthcare provider. Additionally, excessive use of substances like caffeine and alcohol can interfere with the body’s ability to absorb calcium, further contributing to bone loss. Moderation is key, and in some cases, medication may be prescribed to protect bone health, such as bisphosphonates or hormone replacement therapy (HRT) for postmenopausal women.
Understanding and managing these risk factors can help maintain bone health and reduce the risk of osteoporosis, particularly during and after menopause. It is essential to adopt a holistic approach that includes lifestyle modifications, dietary improvements, and medical interventions when necessary. Regular health check-ups and bone density testing can help identify osteoporosis early, allowing for timely and effective management.
Symptoms and Diagnosis of Osteoporosis
The Silent Nature of Osteoporosis
Osteoporosis is often referred to as a “silent disease” because it can progress undetected for many years without symptoms. The first indication of osteoporosis is typically a fracture resulting from a minor fall or, in some cases, no apparent trauma at all. These fractures most commonly occur in the spine, hip, or wrist. The silent progression of the disease underscores the importance of proactive screening and prevention, especially for those at higher risk, such as postmenopausal women.
Importance of Bone Density Testing
Bone Mineral Density (BMD) testing is the primary tool used to diagnose osteoporosis. This non-invasive test measures the density of minerals, such as calcium, in your bones using a technology called Dual Energy X-ray Absorptiometry (DXA). The results are compared to the bone density of a healthy young adult and are reported in the form of a T-score. A T-score of -1.0 or above is considered normal; a T-score between -1.0 and -2.5 indicates low bone mass, or osteopenia; and a T-score of -2.5 or below is diagnostic for osteoporosis. Regular BMD tests can help monitor changes in bone density over time and assess the effectiveness of treatment plans.
When to Consult a Doctor
It is crucial to consult a healthcare provider if you are at risk for osteoporosis, particularly if you are a woman approaching or past menopause. Risk factors include a family history of osteoporosis, early menopause, a thin or small frame, certain medications, and lifestyle factors such as smoking or excessive alcohol consumption. Additionally, if you experience a fracture after a minor incident, height loss, a change in posture, or sudden back pain, these may be signs of osteoporosis and warrant immediate medical attention. Early diagnosis and treatment are vital for maintaining bone health and preventing further bone loss.
Understanding the symptoms and diagnosis of osteoporosis is essential for early intervention and management. By recognizing the silent nature of the disease, the importance of bone density testing, and knowing when to seek medical advice, individuals can take proactive steps towards preserving their bone health and reducing the risk of fractures.
Natural Management of Osteoporosis
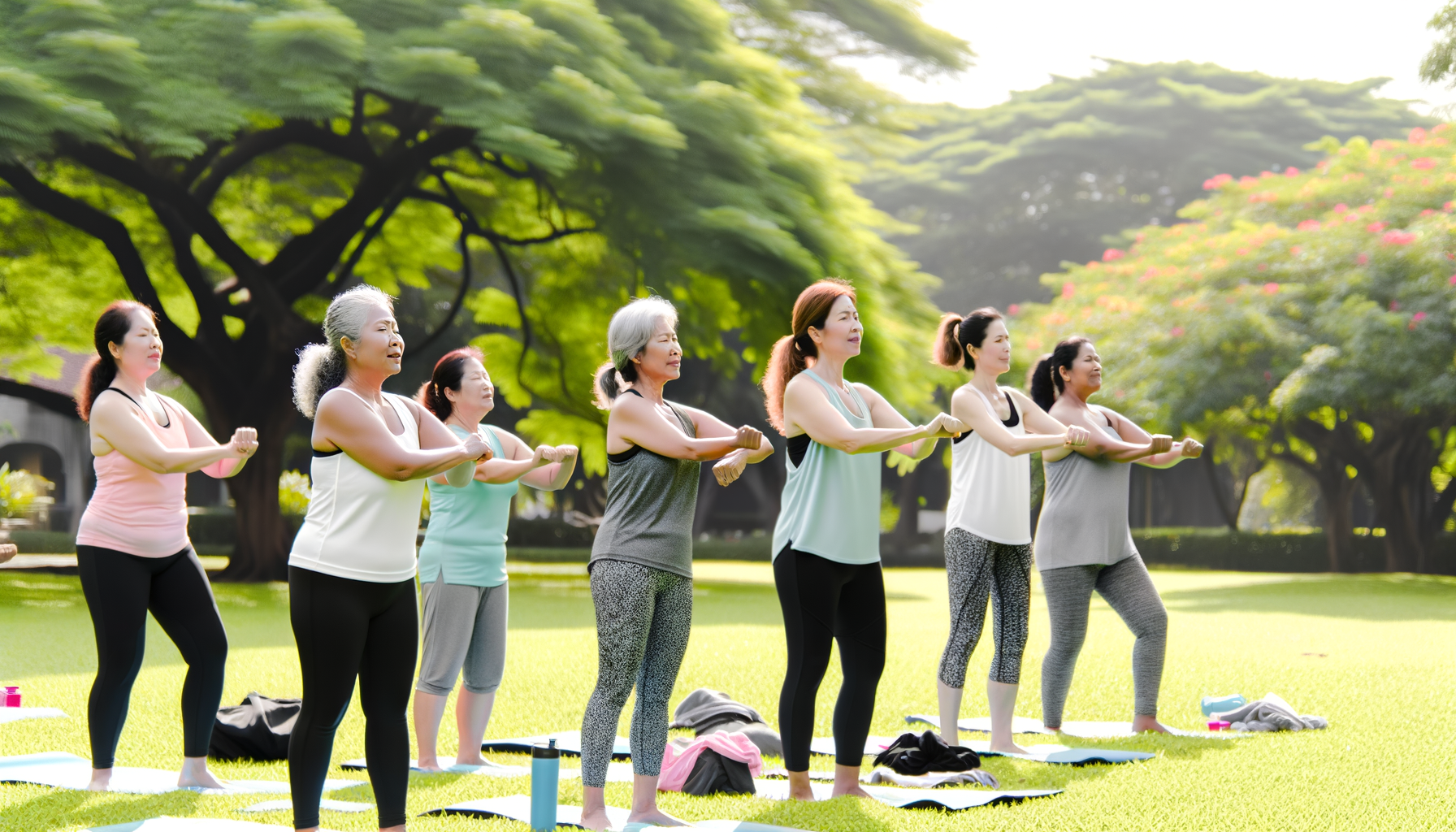
Weight-Bearing and Strength Training Exercises
One of the cornerstones of natural management for osteoporosis is engaging in regular weight-bearing and strength training exercises. These activities help build and maintain bone density by stimulating bone formation. Weight-bearing exercises, such as walking, jogging, and climbing stairs, force the body to work against gravity. Strength training, using free weights, resistance bands, or body weight, further enhances muscle mass, which is crucial for supporting and protecting the skeletal structure. It is recommended to perform these exercises for 30 to 40 minutes on most days of the week, but it’s important to consult with a healthcare professional before starting any new exercise regimen.
Balance Exercises and Fall Prevention
Improving balance is essential in the natural management of osteoporosis, as it helps reduce the risk of falls that could lead to fractures. Balance exercises such as Tai Chi, yoga, and simple activities like standing on one leg can significantly improve stability and coordination. Additionally, creating a safe living environment by removing tripping hazards, installing grab bars, and ensuring adequate lighting can further prevent falls.
Nutritional Support for Bone Health
Adequate nutrition plays a pivotal role in bone health. A diet rich in calcium and vitamin D is vital for maintaining strong bones. Calcium can be found in dairy products, leafy green vegetables, and fortified foods, while vitamin D is synthesized in the skin through sunlight exposure and can be obtained from fatty fish and fortified foods. Other important nutrients include magnesium, which works in tandem with calcium, and vitamin K, which is necessary for bone mineralization. It’s essential to consume a balanced diet that includes these nutrients to support bone health naturally.
The Role of Supplements in Preventing Bone Loss
When dietary intake is insufficient, supplements can play a role in preventing bone loss. Calcium and vitamin D3 supplements are commonly recommended for individuals who may not get enough from their diet or have limited sun exposure. However, it’s crucial to discuss with a healthcare provider before starting any supplementation, as excessive intake can have adverse effects. Other supplements that may support bone health include magnesium, vitamin K, and potentially herbal supplements like red clover and turmeric, though more research is needed to confirm their efficacy.
In conclusion, managing osteoporosis naturally involves a multifaceted approach that includes exercise, fall prevention strategies, proper nutrition, and the judicious use of supplements. By incorporating these elements into daily life, individuals can work towards maintaining bone density and reducing the risk of fractures associated with osteoporosis.
By the way, something for you, a little gift!!!
I am just in the middle of publishing my book. It’s about How women can balance their hormones. One part is about food and diet, of course.
Follow this link and enter your email.
I will send you this part of the book for free once the book is published. It has many concrete, practical tips and recipes and will help you feel better during menopause or times of Big hormonal fluctuations.
Annette, Damiva Lead for Health & Wellness

Nutritional Considerations for Bone Health
Calcium-Rich Foods and Absorption
Calcium is the cornerstone of bone health. Postmenopausal women are recommended to consume at least 1,300 mg of calcium daily, which can be found in dairy products like yogurt, cheese, and milk. Non-dairy sources include firm tofu, almonds, Brazil nuts, and dark green leafy vegetables. Fish with edible bones, such as sardines, also offer a significant amount of calcium. However, the body’s ability to absorb calcium depends on the presence of vitamin D, which is why these two nutrients are often discussed in tandem.
Vitamin D and Its Sources
Vitamin D is essential for calcium absorption and bone health. It is synthesized in the skin through sun exposure and is present in small amounts in foods like fatty fish, egg yolks, and fortified products. The recommended daily intake of vitamin D is 800 IU, but many people, especially those in less sunny climates, may require supplements to achieve optimal levels. A simple blood test can determine if supplementation is necessary.
Magnesium’s Partnership with Calcium
Magnesium works closely with calcium to support bone health. It helps convert vitamin D into its active form, which in turn enhances calcium absorption. Foods rich in magnesium include nuts, seeds, whole grains, and green leafy vegetables. Ensuring an adequate intake of magnesium can support the body’s use of calcium and contribute to bone density maintenance.
Reducing Caffeine and Alcohol Intake
Excessive consumption of caffeine and alcohol can have a negative impact on bone health. Caffeine can interfere with calcium absorption, and high alcohol intake is linked to an increased risk of bone loss and fractures. Moderation is key, and it is advisable for postmenopausal women to limit their intake of these substances to support their bone health.
Phosphorus and Its Effects on Bones
Phosphorus is another mineral important for bone structure, but its balance with calcium is crucial. High phosphorus intake, often from processed foods and soft drinks, can disrupt the calcium-to-phosphorus ratio and potentially lead to bone loss. A diet focusing on natural, nutrient-rich foods will help maintain the proper balance of these minerals.
By considering these nutritional factors, postmenopausal women can take proactive steps to support their bone health and reduce the risk of osteoporosis.
Medical Interventions and Treatments
Hormone Replacement Therapy (HRT) and Its Risks
Hormone Replacement Therapy (HRT) has been a common treatment for the symptoms of menopause and for the prevention of postmenopausal osteoporosis. HRT works by replenishing estrogen, which decreases sharply during menopause, leading to a reduction in bone density. While HRT can be effective in preventing bone loss and fractures, it is not without risks. The Women’s Health Initiative (WHI) study in 2001 highlighted an increased risk of heart attacks, strokes, and breast cancer in women undergoing HRT. Although these risks are relatively small, they have led to a decline in the use of HRT. Subsequent analyses have shown that estrogen alone may be safer than combined estrogen and progestin therapy, and may even reduce the risk of breast cancer.
Alternative Medications and Therapies
Bisphosphonates have become the mainstay of osteoporosis treatment over the past 15 years. These drugs, such as alendronate and risedronate, reduce fracture rates by about 50 percent and are generally well tolerated. Newer therapies based on a deeper understanding of bone biology are being developed, including Denosumab, an antibody that blocks bone resorption, and medications targeting sclerostin, which shows promise in increasing bone density.
Monitoring and Adjusting Treatment Plans
Effective management of osteoporosis involves regular monitoring of bone density through DXA scans and adjusting treatment plans accordingly. The FRAX tool can help estimate a patient’s 10-year fracture risk, guiding decisions about when to initiate or adjust therapy. For those on bisphosphonates, a “drug holiday” may be considered after several years of treatment, although the optimal duration of therapy and timing of such breaks are still under investigation. It is crucial to reassess fracture risk periodically, especially after discontinuing treatments like Denosumab, which may lead to rapid bone loss upon cessation.
In conclusion, while HRT may be beneficial for bone health, especially in younger postmenopausal women, alternative medications like bisphosphonates and newer biological therapies offer effective options for managing osteoporosis. Regular monitoring and personalized treatment strategies are key to optimizing bone health and reducing the risk of fractures.
Conclusion: Proactive Bone Health Management
The Importance of Early Intervention
Early intervention in bone health is crucial for preventing osteoporosis and related fractures. The foundation for strong bones is laid early in life, with peak bone mass typically achieved by the late twenties. Engaging in bone-strengthening activities, ensuring adequate nutrition, and avoiding lifestyle choices that negatively impact bone density are essential steps that should begin in childhood and continue throughout adolescence and adulthood. Early screening, particularly around the time of menopause, can identify individuals at risk and facilitate timely management strategies to preserve bone health.
Creating a Personalized Bone Health Strategy
Each individual’s journey to maintaining bone health is unique, influenced by genetic predisposition, lifestyle choices, and medical history. A personalized bone health strategy should be developed in consultation with healthcare providers, taking into account factors such as age, sex, ethnicity, family history, and the presence of risk factors beyond menopause. This strategy may include a combination of dietary adjustments, exercise regimens, lifestyle modifications, and, when appropriate, pharmacological interventions. Regular monitoring and adjustments to the strategy ensure it remains effective over time.
- Weight-bearing exercises: Activities that force you to work against gravity, such as walking and lifting weights, are particularly beneficial for bone health.
- Nutritional adjustments: A diet rich in calcium and vitamin D is vital for bone health. Foods such as dairy products, leafy greens, and fortified foods contribute to the required daily intake.
- Lifestyle modifications: Quitting smoking and reducing alcohol consumption can have a positive impact on bone density.
- Pharmacological interventions: In some cases, medications may be prescribed to prevent bone loss or increase bone density.

Encouraging Regular Health Check-Ups
Regular health check-ups play a pivotal role in proactive bone health management. These check-ups provide an opportunity for healthcare providers to assess bone density, discuss potential concerns, and modify management strategies as needed. Bone density testing, such as dual-energy X-ray absorptiometry (DXA), is a critical tool for diagnosing osteoporosis and should be utilized according to individual risk profiles. Encouraging patients to maintain a schedule of regular health check-ups fosters a proactive approach to bone health, ultimately reducing the risk of osteoporosis and fractures.
In conclusion, proactive management of bone health is essential for preventing osteoporosis and minimizing the risk of fractures. Early intervention, personalized strategies, and regular health check-ups are key components of an effective bone health management plan. By prioritizing bone health throughout life, individuals can maintain stronger bones and a better quality of life as they age.