Menopause marks the end of a woman’s reproductive years, signifying the cessation of menstruation and the ability to conceive naturally. This biological transition typically occurs between the ages of 45 and 55, with the average onset at 51 years in the United States. Menopause is preceded by perimenopause, a transitional phase that can last several years, during which women may experience irregular menstrual cycles and fluctuations in hormone levels. The decline in estrogen and progesterone production by the ovaries during this period leads to the eventual end of menstrual periods and the onset of menopause.
Common Symptoms and Quality of Life Issues
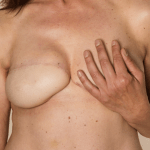
Menopause and perimenopause are associated with a variety of symptoms that can significantly impact a woman’s quality of life. Common symptoms include hot flashes, night sweats, mood swings, sleep disturbances, and vaginal dryness. These changes can affect physical comfort, emotional well-being, and sexual health. The reduction in estrogen levels is also linked to long-term health risks such as osteoporosis and cardiovascular disease. The severity and duration of menopausal symptoms vary widely among women, with some experiencing minimal discomfort and others facing substantial challenges.
The Potential of Ovarian Tissue Freezing
Ovarian tissue freezing, also known as ovarian tissue cryopreservation, has emerged as a promising technique with the potential to delay or even prevent menopause. Initially developed as a fertility preservation method for women undergoing treatments that could harm their reproductive organs, such as chemotherapy, this procedure involves the removal, freezing, and storage of ovarian tissue. Upon reimplantation, the tissue can restore hormonal function and fertility. Recent advancements suggest that ovarian tissue freezing could also be used to prolong reproductive lifespan and delay the onset of menopause, offering a new frontier in women’s health management.
The Science Behind Ovarian Tissue Freezing
Overview of Ovarian Tissue Cryopreservation
Ovarian tissue cryopreservation, also known as ovarian tissue freezing, is a fertility preservation technique that involves the removal and storage of ovarian tissue at very low temperatures. This process aims to safeguard a woman’s reproductive potential, particularly in cases where medical treatments, such as chemotherapy, may compromise fertility. The tissue, which contains thousands of dormant eggs, can later be thawed and reimplanted to restore fertility or delay menopause.
The Process of Ovarian Tissue Transplant
The process of ovarian tissue transplant begins with the laparoscopic removal of ovarian tissue, which is then sliced into thin strips and frozen using cryoprotectants to prevent ice crystal formation and cellular damage. When a woman is ready to restore her fertility or delay menopause, the tissue is thawed and transplanted back into her body. The tissue can be placed near the remaining ovarian tissue or in an alternative site, such as under the skin, where it can reestablish a blood supply and resume function.
Advancements in Cryopreservation Techniques
Advancements in cryopreservation techniques have significantly improved the success rates of ovarian tissue freezing and transplantation. Innovations include the development of more effective cryoprotectants and protocols that minimize damage to the ovarian tissue during the freezing and thawing processes. Additionally, research into enhancing the revascularization of transplanted tissue aims to reduce the loss of primordial follicles post-transplant. These improvements are crucial for increasing the viability of the tissue and the longevity of its function once reimplanted.
While ovarian tissue freezing offers hope for extending reproductive lifespan and managing menopause, it is still considered experimental and is not without risks. The procedure’s success depends on various factors, including the patient’s age at the time of tissue harvest, the amount of tissue collected, and the survival rate of follicles after transplantation. As the science continues to evolve, ovarian tissue freezing may become a more accessible and reliable option for women seeking to preserve their fertility and hormonal health.
Research Findings and Predictive Modeling
Study Outcomes on Delaying Menopause
Recent advancements in ovarian tissue cryopreservation and transplant (OTCT) have opened new avenues for potentially delaying the onset of menopause. A mathematical modeling study published in the American Journal of Obstetrics and Gynecology suggests that by removing, freezing, and later reimplanting ovarian tissue, the fertile years can be extended beyond the typical age of menopause. The model incorporated data from previous studies on ovarian reserve at different ages and the behavior of ovarian follicles in tissue. It predicted that for most women under 40, OTCT could significantly delay menopause. The success of the transplant depended on several factors, including the age at ovarian tissue harvest, the amount of tissue harvested, and the proportion of follicles that survived post-transplant.
Factors Influencing the Success of Transplants
The success of ovarian tissue transplants is influenced by multiple factors:
- Age at ovarian tissue harvest: Tissue harvested before the age of 40 showed a higher potential for delaying menopause due to a larger number of viable follicles.
- Amount of ovarian tissue harvested: The quantity of tissue is critical; too little may not delay menopause, while too much could induce early menopause. The model provided an optimum amount for harvesting based on age.
- Single vs. Multiple transplants: Dividing the tissue and performing multiple transplants could extend the delay of menopause. For instance, three transplants could extend the delay to 23 years, and six transplants to 31 years.
- Follicle survival rate: The model indicated that a higher survival rate of follicles post-transplant could lead to a more significant delay in menopause.
Limitations and Considerations in Current Research
While the predictive model offers promising insights, its practical utility is currently limited. The model’s predictions are based on the assumption of technological advancements that could improve follicle survival rates. Additionally, ethical and personal considerations must be taken into account, as menopause is a natural stage of life and not a disease. The potential benefits of delaying menopause, such as reduced risks of osteoporosis and cardiovascular disease, must be weighed against the increased risks of certain cancers. Furthermore, the technique involves repeated surgeries, which carry inherent risks. Current research also does not fully address the long-term health implications of significantly delaying menopause.
Overall, while OTCT has shown promise in preserving fertility and restoring endocrine function, particularly after cancer treatments, its application solely for delaying menopause requires further investigation. The broader impact on women’s health, quality of life, and societal perspectives must be thoroughly evaluated before such procedures can be recommended for delaying menopause.
Clinical Applications and Patient Considerations
Fertility Restoration After Cancer Treatments
Ovarian tissue freezing, also known as ovarian tissue cryopreservation, has emerged as a beacon of hope for cancer patients whose treatments pose a risk to their fertility. This technique involves the laparoscopic removal of ovarian tissue prior to initiating cancer therapy, which is known to potentially compromise ovarian function. The tissue, rich in primordial follicles, is then cryogenically preserved. Post-treatment, the tissue can be thawed and reimplanted, with the aim of restoring not only fertility but also endocrine function. This has profound implications, as it offers the possibility of conceiving naturally and experiencing the natural menstrual cycles that contribute to a woman’s overall health and well-being. The success of such transplants has been documented, with a significant number of women achieving pregnancy and childbirth, thereby addressing a critical quality of life issue for cancer survivors.
Ethical and Personal Considerations
The prospect of delaying or preventing menopause through ovarian tissue freezing raises a myriad of ethical and personal considerations. Ethically, the manipulation of a natural life stage such as menopause prompts discussions about the medicalization of female aging and the societal pressures on women’s reproductive choices. Personally, women must weigh the potential long-term health benefits against the risks and costs associated with the procedure. The decision to undergo ovarian tissue freezing is deeply personal, often influenced by factors such as the desire for biological children, family history of early menopause, or the presence of conditions exacerbated by the loss of ovarian hormones.
Risks and Benefits of Delaying Menopause
Delaying menopause through ovarian tissue freezing presents a complex balance of risks and benefits. On the one hand, extending the reproductive lifespan can have positive health implications, such as reduced risks of osteoporosis, cardiovascular disease, and other conditions associated with estrogen deficiency. On the other hand, prolonged exposure to endogenous hormones may increase the risk of hormone-sensitive cancers. Furthermore, the psychological impact of extending fertility potential into later life stages and the societal implications of shifting the natural timeline of reproduction warrant careful consideration. Patients must be counseled on these potential outcomes to make informed decisions that align with their personal health goals and ethical beliefs.
Alternative Approaches to Managing Menopause
Menopausal Hormone Therapy (MHT)
Menopausal Hormone Therapy, commonly known as hormone replacement therapy (HRT), has been a traditional approach to managing the symptoms of menopause. MHT involves the administration of estrogen or a combination of estrogen and progesterone to alleviate common menopausal symptoms such as hot flashes, night sweats, and vaginal dryness. While MHT can significantly improve quality of life for many women, it is not without risks. Studies have linked long-term use of certain types of MHT to an increased risk of breast cancer, heart disease, stroke, and blood clots. Consequently, MHT is typically recommended at the lowest effective dose for the shortest duration necessary.
Lifestyle and Non-Hormonal Interventions
For women who prefer not to use hormone therapy or for whom it is contraindicated, there are several non-hormonal interventions that can help manage menopausal symptoms. These include lifestyle modifications such as regular exercise, maintaining a healthy diet, and ensuring adequate sleep. Additionally, non-hormonal medications like selective serotonin reuptake inhibitors (SSRIs) and gabapentin have been shown to reduce hot flashes. Complementary therapies such as acupuncture, yoga, and mindfulness meditation may also provide relief for some women.
Comparing MHT with Ovarian Tissue Freezing
Ovarian tissue freezing, a newer technique, offers an alternative to traditional MHT by preserving a woman’s own ovarian tissue, which can later be transplanted to delay menopause and extend fertility. Unlike MHT, which introduces hormones externally, ovarian tissue transplants could potentially allow for natural hormone production. This method could circumvent the risks associated with synthetic hormones, though it is not without its own set of challenges, including surgical risks and the uncertainty of long-term outcomes. Moreover, ovarian tissue freezing is currently an expensive and specialized procedure not accessible to all women.
While ovarian tissue freezing presents an intriguing option, it is still considered experimental and is primarily used for fertility preservation in women undergoing treatments that could damage their ovaries. As research progresses, it may become a viable option for delaying menopause, but for now, MHT remains the most established method for managing menopausal symptoms, with lifestyle and non-hormonal interventions serving as important adjuncts or alternatives.
The Broader Impact of Delaying Menopause
Health Benefits and Risks
Delaying menopause through ovarian tissue freezing presents a complex interplay of potential health benefits and risks. On the one hand, later onset of natural menopause has been associated with a longer lifespan and reduced risk for various conditions, including cardiovascular disease, osteoporosis, and certain neurodegenerative diseases. The preservation of ovarian function via tissue freezing could, hypothetically, extend these benefits to women who undergo the procedure. However, it is crucial to recognize that the relationship between delayed menopause and health outcomes is not fully understood, and the long-term effects of artificially extending reproductive lifespan are yet to be determined.
Societal and Individual Perspectives
From a societal standpoint, the ability to delay menopause could have profound implications. It challenges traditional views of aging and could shift societal norms regarding the timing of childbearing, career planning, and retirement. Individually, women may face complex decisions about their reproductive health and personal life trajectories. While some may welcome the opportunity to extend fertility, others may question the medicalization of a natural life stage and the potential pressure to maintain reproductive capacity for longer.
The Future of Menopause Management
The prospect of delaying or preventing menopause through ovarian tissue freezing opens new frontiers in menopause management. As research progresses, we may see a paradigm shift where menopause becomes a more controllable aspect of women’s health. This could lead to personalized approaches to reproductive aging, with interventions tailored to individual health profiles and life plans. However, such advancements also necessitate careful ethical considerations, regulatory oversight, and equitable access to ensure that the benefits of this technology are available to all women, not just a privileged few.
In conclusion, while the potential to delay or prevent menopause through ovarian tissue freezing is an exciting scientific development, it is accompanied by a host of medical, ethical, and societal considerations that must be thoughtfully addressed. The future of menopause management may indeed be on the cusp of significant change, but it is imperative that such change is guided by a commitment to improving women’s health and well-being across the lifespan.

Popular Read
Conclusion and Future Directions
Ovarian tissue freezing, a pioneering technique in the realm of fertility preservation, has emerged as a beacon of hope for women facing the loss of reproductive function due to medical treatments or premature ovarian failure. The process, which involves the cryopreservation of ovarian tissue and its subsequent transplantation, has the potential to not only restore fertility but also to extend the reproductive lifespan and delay the onset of menopause. This innovative approach has been successfully utilized to enable cancer survivors to conceive and give birth, highlighting its efficacy in preserving and restoring ovarian function.
Remaining Questions and Areas for Further Research
Despite the promising outcomes, several questions remain unanswered, necessitating further research. The efficiency of primordial follicle survival post-cryopreservation and transplantation is a critical area of study, as is the impact of ovarian tissue harvesting on the natural age of menopause. Additionally, the long-term health implications of restoring ovarian endocrine function through autotransplantation, particularly in comparison to traditional hormone replacement therapy, require thorough investigation. The ethical considerations surrounding the elective use of ovarian tissue freezing for non-medical purposes also warrant careful scrutiny.
- How effectively does the primordial follicle reserve survive post-transplantation?
- Can the duration of reproductive life reduced by ovarian tissue removal be matched or exceeded by the length of endocrine function gained after autotransplantation?
- What is the minimum amount of ovarian tissue that can be safely harvested without inducing earlier menopause?
- What are the best practices for cryopreserving, thawing, and transplanting ovarian tissues to achieve maximum longevity and success?
Empowering Women with Knowledge and Choices
The advent of ovarian tissue freezing offers women unprecedented control over their reproductive health and life choices. By providing women with comprehensive information on the risks, benefits, and alternatives to ovarian tissue freezing, healthcare providers can empower them to make informed decisions that align with their personal and reproductive goals. As research continues to advance, it is imperative to ensure that women are equipped with the knowledge to navigate the evolving landscape of fertility preservation and menopause management.
In conclusion, ovarian tissue freezing stands at the forefront of reproductive medicine, offering the potential to revolutionize the way we approach fertility preservation and menopause. As we move forward, it is crucial to address the remaining questions through rigorous research, to refine the techniques involved, and to empower women with the knowledge and choices they need to take charge of their reproductive futures.