Sugar and Gut Health
Sugar has become a staple in modern diets, with its presence felt in a wide array of foods and beverages. The United States leads the world in sugar consumption, with the average American adult consuming over 15 teaspoons of sugar per day, significantly exceeding the American Heart Association’s recommended daily amount of 9 teaspoons for men and 6 teaspoons for women. This excessive intake is linked to a plethora of health issues, including obesity, heart disease, type 2 diabetes, and various forms of cancer. However, the impact of sugar extends beyond these well-known conditions, affecting the delicate balance of the gut microbiome, which is essential for overall health.
Purpose of the Article
The aim of this article is to explore the relationship between sugar consumption and gut health. We will delve into the science behind how sugar affects the trillions of microorganisms residing in our gastrointestinal tract and the subsequent consequences on our well-being. By examining the latest research and expert insights, we aim to provide a comprehensive understanding of the implications of sugar on gut health and offer guidance on how to maintain a healthy gut microbiome.
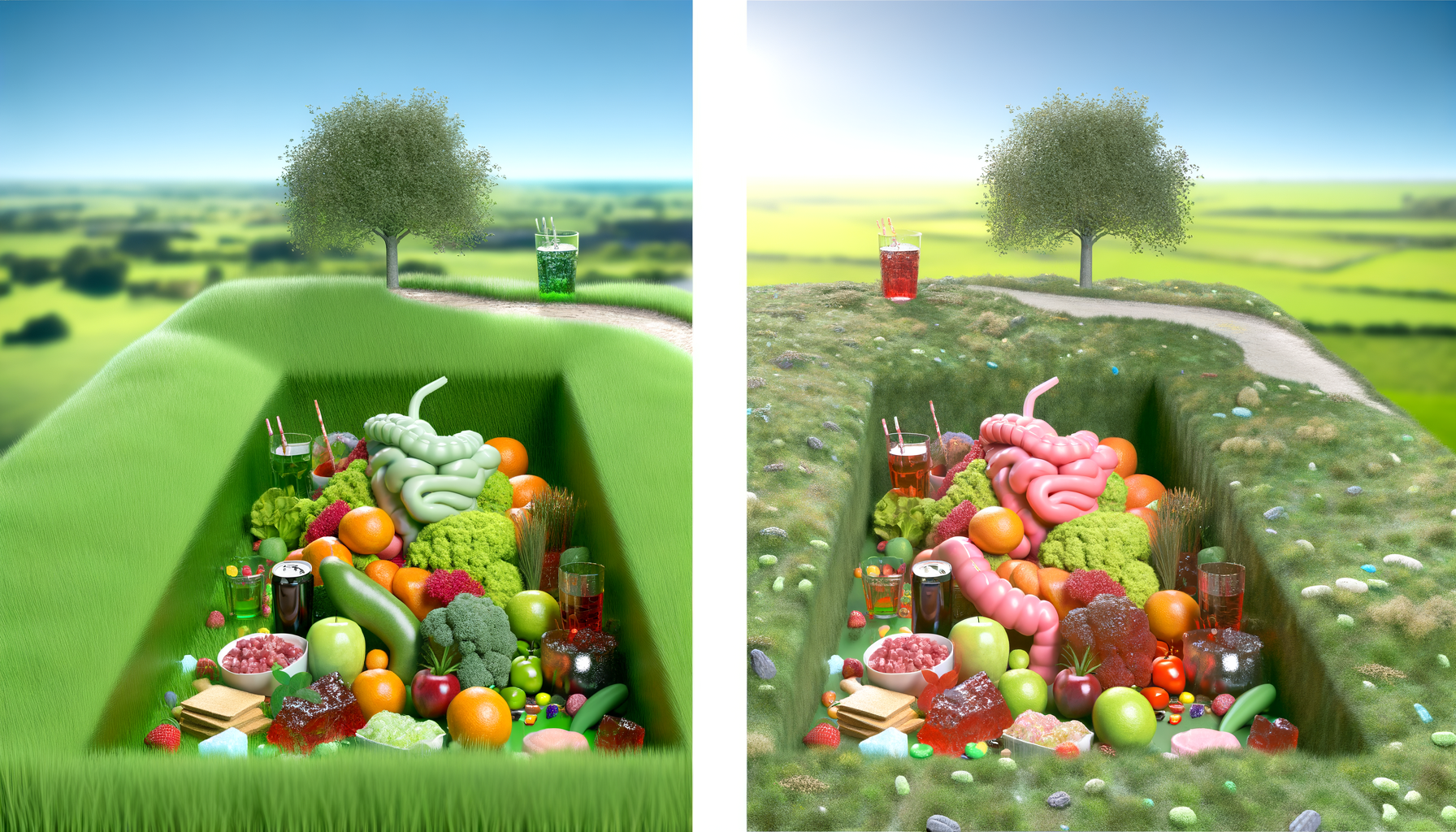
Overview of Sugar’s Impact on Gut Health
Recent studies have shed light on the profound impact that a high-sugar diet can have on the gut microbiota. For instance, research published in the journal Cell revealed that mice on a high-sugar, high-fat diet experienced significant changes in their gut bacteria over a four-week period. Notably, the abundance of segmented filamentous bacteria (SFB), which play a crucial role in maintaining the gut immune system, plummeted. This led to a reduction in Th17 immune cells, which are vital for protecting the gut from inflammation and pathogenic lipids. While these findings cannot be directly applied to humans, they underscore the importance of a balanced gut flora for health. Furthermore, excessive sugar intake may promote bacteria that erode the gut’s protective mucus layer, increasing the risk of conditions like ulcerative colitis. The protective role of dietary fiber, which can counteract the negative effects of sugar, will also be discussed, highlighting the importance of a varied diet rich in fruits, vegetables, and fiber for optimal gut health.
Understanding the Gut Microbiome
The gut microbiome is a complex and dynamic ecosystem, housing trillions of microorganisms, including bacteria, viruses, fungi, and protozoa. These microorganisms reside primarily in the large intestine and play a pivotal role in human health. They are involved in various functions such as digestion, vitamin production, and the development of the immune system. The gut microbiota helps break down complex carbohydrates and fibers that our own digestive enzymes cannot handle, producing short-chain fatty acids that nourish the gut lining. Additionally, they synthesize essential vitamins like vitamin K and some B vitamins.
The Importance of Microbial Diversity
Microbial diversity is a hallmark of a healthy gut microbiome. A diverse microbial population is associated with greater resilience and stability of the gut ecosystem, which can better withstand disturbances like dietary changes or antibiotic use. High microbial diversity is linked to a reduced risk of conditions such as obesity, type 2 diabetes, and inflammatory bowel diseases. It ensures a wide range of functional capabilities that contribute to the metabolic, nutritional, and immune functions of the host.
Gut Microbiome and Overall Health
The gut microbiome’s influence extends beyond the digestive system, impacting overall health. It interacts with the body’s immune system to train it to distinguish between harmful and benign invaders. This interaction is crucial for maintaining immune homeostasis and preventing autoimmune diseases. The gut-brain axis, a bidirectional communication pathway between the gut and the brain, suggests that the gut microbiota can influence mood, behavior, and cognitive functions. Moreover, a balanced gut microbiome is associated with a lower risk of developing metabolic diseases, such as obesity and type 2 diabetes, and plays a role in cardiovascular health.
In summary, the gut microbiome is an intricate community that is essential for digestion, immune function, and overall well-being. Its composition and diversity are critical for its proper function, and maintaining a balanced gut microbiome is vital for good health.

THEN IT CONTAINS TOXIC CHEMICALS. WHY RISK IT GETTING SICK? GO CHEMICAL FREE.
The Effects of Sugar on the Gut Microbiota
The modern Western diet, characterized by high consumption of processed foods and sugars, has been linked to a disruption in the delicate balance of the gut microbiome. Studies in both humans and animal models have shown that diets rich in sugar can lead to significant changes in the composition and functionality of gut bacteria. One of the primary ways that high-sugar diets disrupt microbial balance is by decreasing bacterial diversity, which is a key indicator of a healthy gut microbiome. This reduction in diversity can pave the way for an overgrowth of certain bacteria that thrive on simple sugars, such as members of the Proteobacteria phylum, at the expense of other beneficial microbes.
Specific Changes in Gut Bacteria Due to Sugar
Research has identified specific changes in gut bacteria populations due to high sugar intake. For instance, a decrease in the abundance of Bacteroidetes and an increase in Proteobacteria have been observed. These shifts are concerning because Proteobacteria include many species known to induce inflammation and are often associated with various diseases. Conversely, Bacteroidetes are typically considered beneficial as they are involved in complex carbohydrate breakdown and the production of short-chain fatty acids, which are important for gut health. The loss of these beneficial microbes and the overrepresentation of potentially harmful ones can lead to a state of dysbiosis, where the gut ecosystem becomes imbalanced and less capable of supporting health.
Consequences of a High-Sugar Diet on Gut Health
The consequences of a high-sugar diet on gut health are multifaceted and can have far-reaching effects on overall well-being. One of the most immediate impacts is the alteration of the gut’s immune response. For example, a reduction in segmented filamentous bacteria (SFB) can lead to a decrease in Th17 immune cells, which play a crucial role in maintaining gut barrier integrity and preventing inflammation. Without these immune cells, the gut becomes more susceptible to the absorption of pathogenic lipids and the development of intestinal inflammation.
Furthermore, the imbalance caused by a high-sugar diet can increase gut permeability, sometimes referred to as “leaky gut,” allowing bacterial lipopolysaccharide (LPS) to enter the bloodstream. This condition, known as metabolic endotoxemia, can trigger systemic inflammation and contribute to the development of metabolic disorders such as obesity and type 2 diabetes, even in the absence of weight gain. The shift towards a pro-inflammatory state in the gut also has implications for the development of inflammatory bowel diseases (IBD) and other chronic conditions.
In conclusion, the evidence suggests that high-sugar diets can lead to significant disruptions in the gut microbiota, with potential consequences that include increased inflammation, compromised gut barrier function, and a heightened risk for metabolic and inflammatory diseases. As such, moderating sugar intake and maintaining a diet rich in diverse, fiber-filled foods is essential for preserving gut health and overall well-being.
Do you know the three main ways that your body gets in touch with harmful chemicals with everyday products? Knowledge is Power!
The Ultimate Detox Guide will tell you how to lower your exposure to harmful chemicals!

Sugar Consumption: Recommended Intake vs. Reality
The modern diet is saturated with sugar, often exceeding the recommended daily intake. The average American consumes approximately 17 teaspoons (tsp) of added sugars per day, which is significantly higher than the American Heart Association’s recommendations of no more than 6 tsp for women and 9 tsp for men. This excessive consumption is facilitated by the prevalence of high-fructose corn syrup (HFCS) in soft drinks and processed foods, even those perceived as “healthy” options like sweetened yogurt and granola bars.
Health Guidelines on Sugar Intake
Health organizations have established guidelines to curb sugar intake due to its association with various health issues, including obesity, type 2 diabetes, and heart disease. The Dietary Guidelines for Americans suggest that added sugars should not exceed 10% of total daily calories. For a 2,000 calorie diet, this equates to about 50 grams or 13 tsp of added sugar. However, a single 12-ounce can of soda can contain nearly 8 tsp of added sugar, illustrating the ease with which one can surpass these limits.
The Gap Between Recommendations and Actual Intake
Despite clear guidelines, there is a significant gap between recommended sugar intake and actual consumption. This discrepancy is partly due to the hidden sugars in many processed foods and the lack of public awareness. For instance, consumers may not realize that “natural” or “healthy” labeled products can still be high in added sugars. The challenge is further compounded by the food industry’s use of alternative sweeteners and sugar by different names, which can mislead and make it difficult for consumers to recognize sugar content.
Efforts to reduce sugar intake are essential for improving gut health and overall well-being. Strategies such as reading nutrition labels carefully, choosing whole foods over processed ones, and being mindful of the various names for sugar can help bridge the gap between recommended intake and reality. Additionally, simple dietary changes like replacing sugary beverages with water or unsweetened alternatives can significantly reduce sugar consumption and support a healthier gut microbiome.
Scientific Insights: Sugar’s Impact on Gut Health
Animal studies have been instrumental in uncovering the effects of sugar on gut health. Research involving rodents has shown that diets high in sugars such as fructose and glucose can lead to gut dysbiosis, characterized by a decrease in microbial diversity and an imbalance in the gut microbiota composition. For instance, mice fed with high-glucose diets exhibited hyperglycemia, glucose intolerance, and increased fat mass deposition, alongside a reduction in beneficial Bacteroidetes and an increase in potentially harmful Proteobacteria. These dietary patterns also resulted in increased gut permeability and inflammation, suggesting a link between sugar intake and compromised gut barrier function.
Human Studies and Observational Data
Human studies, although less conclusive due to their observational nature, have provided insights into the relationship between sugar consumption and gut health. Excessive intake of added sugars has been associated with conditions such as obesity, type 2 diabetes, and cardiovascular disease, which are also linked to alterations in the gut microbiome. However, the specific effects of sugar on the human gut microbiota are challenging to isolate due to the complexity of dietary patterns and individual variations in microbiome composition. Despite these challenges, some studies have indicated that high sugar diets may reduce microbial diversity and favor the proliferation of pathogenic bacteria.
The Protective Role of Dietary Fiber
Contrasting the detrimental effects of high-sugar diets, dietary fiber plays a protective role in maintaining gut health. Fiber-rich foods promote the growth of beneficial gut bacteria and the production of short-chain fatty acids (SCFAs), which are crucial for maintaining the integrity of the gut barrier and exerting anti-inflammatory effects. Animal studies have shown that diets high in fiber can mitigate the negative impacts of sugar on the gut microbiota, highlighting the importance of a balanced diet for gut health.
In conclusion, while animal studies have provided strong evidence of sugar’s adverse effects on gut health, human studies are still evolving. The protective role of dietary fiber is well-established, emphasizing the need for dietary strategies that balance sugar intake with adequate fiber consumption to support a healthy gut microbiome.
By the way, something for you, a little gift!!!
I am just in the middle of publishing my book. It’s about How women can balance their hormones. One part is about food and diet, of course.
Follow this link and enter your email.
I will send you this part of the book for free once the book is published. It has many concrete, practical tips and recipes and will help you feel better during menopause or times of Big hormonal fluctuations.
Annette, Damiva Lead for Health & Wellness

Sugar and Inflammatory Bowel Diseases
The consumption of sugar, particularly in high amounts, has been implicated in a variety of health issues, including obesity, type 2 diabetes, and cardiovascular disease. However, its role in the development and exacerbation of inflammatory bowel diseases (IBD), such as ulcerative colitis (UC), is an area of growing research interest. Studies have suggested that diets high in sugar may contribute to the onset and progression of UC by altering the gut microbiome. For instance, research indicates that a high-sugar diet can lead to an overgrowth of mucus-degrading bacteria, which in turn erodes the gut’s protective mucus layer, potentially setting the stage for colitis. This erosion compromises the intestinal barrier, allowing pathogenic bacteria to trigger an inflammatory response in the gut.
Protective Effects of Vegetables and Fiber
Conversely, the intake of vegetables and dietary fiber appears to offer protective effects against the development of UC. Fiber-rich foods, such as vegetables and fruits, are not only essential for digestive health but also encourage the growth of beneficial gut bacteria. These beneficial bacteria ferment the fiber, producing short-chain fatty acids (SCFAs) like butyrate, which are crucial for maintaining gut health. SCFAs have been shown to play a role in reducing inflammation and promoting the healing of the intestinal lining. Therefore, a diet high in fiber may counteract the harmful effects of sugar on the gut microbiome and help maintain a healthy gut barrier.
Dietary Strategies for Managing IBD Symptoms
For individuals with IBD, dietary management is a key component of symptom control. While high-sugar diets are discouraged, increasing the intake of fiber-rich foods can be beneficial. However, during an IBD flare, some patients may be advised to limit fiber intake to reduce discomfort. In such cases, it is important to find a balance and ensure that the diet does not become too restrictive, as this could lead to nutritional deficiencies. Patients with IBD should work with healthcare professionals, including dietitians, to develop individualized eating plans that manage symptoms while also supporting overall gut health. Strategies may include identifying and avoiding specific triggers, incorporating probiotics, and ensuring adequate nutrition.
In conclusion, while sugar is not the sole cause of IBD, evidence suggests that high-sugar diets can exacerbate gut inflammation and contribute to the development of conditions like UC. Balancing sugar intake with a diet rich in vegetables and fiber can help protect gut health and manage IBD symptoms.

Reevaluating Our Relationship with Sugar
Understanding the difference between natural and added sugars is crucial in reevaluating our relationship with this sweet substance. Natural sugars are found inherently in foods such as fruits (fructose) and dairy products (lactose). They should be avoided but at least they come with essential nutrients, fiber, and water that help mitigate the negative effects of sugar on the body. On the other hand, added sugars are those incorporated into foods during processing or preparation, such as sodas, candies, and baked goods. These sugars contribute to calorie intake without providing any nutritional benefit. They should be cut.
Emotional and Behavioral Aspects of Sugar Consumption
Sugar consumption is not just a physical health issue but also an emotional and behavioral one. The pleasure derived from eating sugary foods can lead to a habitual cycle of cravings and indulgence, similar to other addictive behaviors. This is partly due to the release of dopamine, a neurotransmitter associated with the reward center in the brain. Recognizing the emotional ties to sugar consumption is a step towards developing healthier eating habits and breaking the cycle of sugar dependency.
Strategies for Reducing Sugar in the Diet
- Read Labels: Become familiar with nutrition labels to identify added sugars in products. Look for terms like sucrose, high-fructose corn syrup, and dextrose.
- Start Small: Gradually reduce the amount of sugar you add to foods and drinks. Over time, your taste buds can adjust to enjoy less sweet flavors.
- Choose Whole Foods: Opt for whole fruits instead of fruit juices or sweetened snacks. Whole foods provide fiber and essential nutrients, helping to balance blood sugar levels.
- Spice It Up: Use spices like cinnamon, nutmeg, or vanilla to add flavor without the need for sugar.
Balancing Sugar Intake for Gut Health
In conclusion, while sugar plays a role in our diets, it’s important to strike a balance to maintain gut health and overall well-being. By differentiating between natural and added sugars, understanding the emotional aspects of sugar consumption, and implementing strategies to reduce intake, we can foster a healthier relationship with sugar. This balance is not about complete deprivation but about making informed choices that support our gut microbiome and reduce the risk of health issues associated with high sugar consumption. Embrace a diet rich in diversity, including plenty of protein, non inflammatory plants, and fermented foods, to nourish your body and your gut microbes for optimal health.