Introduction to Perimenopause and Menopause
Defining Perimenopause and Menopause
Perimenopause and menopause mark the end of the reproductive phase in a woman’s life. Perimenopause is the transitional period leading up to menopause, often beginning in a woman’s 40s, but it can start as early as the mid-30s. During this time, the ovaries gradually produce less estrogen, leading to irregular menstrual cycles and various physical and emotional symptoms. Menopause is defined as the point when a woman has not had a menstrual period for 12 consecutive months. It typically occurs between the ages of 45 and 55, but the timing can vary widely.
Physical, Mental, and Emotional Impacts
The journey through perimenopause to menopause can significantly impact a woman’s life. Physically, women may experience hot flashes, night sweats, sleep disturbances, and weight gain. Mentally and emotionally, there may be mood swings, anxiety, depression, and a decrease in cognitive function, often referred to as “brain fog.” These changes can affect personal relationships, professional life, and overall well-being.
Overview of Hormonal Fluctuations
Hormonal fluctuations are at the core of perimenopause and menopause. Estrogen and progesterone levels decline unevenly, leading to the symptoms associated with this life stage. The decrease in estrogen is particularly significant, as it affects various bodily systems, including the cardiovascular, skeletal, and central nervous systems.
Symptoms and Challenges
- Vasomotor symptoms: Hot flashes and night sweats are common and can disrupt daily activities and sleep.
- Menstrual irregularity: Periods may become unpredictable, lighter, or heavier.
- Vaginal and urinary issues: Vaginal dryness, discomfort during intercourse, and urinary incontinence may occur.
- Sexual function: Changes in sexual desire and response can affect intimate relationships.
- Emotional changes: Increased risk of depression, anxiety, and mood swings.
- Cognitive changes: Memory lapses and difficulty concentrating can be frustrating.
- Skeletal health: Accelerated bone loss can increase the risk of osteoporosis and fractures.
Understanding these symptoms and challenges is crucial for women to seek appropriate care and support during this transition.
Blood Sugar Dynamics in Women’s Health
The Role of Blood Sugar in the Body
Blood sugar, or glucose, is the primary source of energy for the body’s cells. It fuels the brain, muscles, and other vital organs. After consuming food, carbohydrates are broken down into glucose, which enters the bloodstream. The pancreas then releases insulin, a hormone that facilitates the uptake of glucose into cells, where it is used for energy or stored for future use.
Importance of Blood Sugar Regulation
Regulating blood sugar levels is crucial for maintaining overall health. Stable blood sugar supports cognitive function, mood stability, and energy levels throughout the day. It also plays a significant role in appetite control, helping to prevent overeating and supporting weight management efforts.
- Consistent Energy: Well-regulated blood sugar provides a steady supply of energy, preventing the highs and lows associated with blood sugar spikes and crashes.
- Hormonal Balance: Blood sugar levels can influence the balance of hormones in the body, including those involved in the menstrual cycle and stress response.
- Metabolic Health: Proper blood sugar regulation is a key factor in metabolic health, reducing the risk of developing conditions such as insulin resistance, prediabetes, and type 2 diabetes.
Consequences of Blood Sugar Imbalance
Imbalances in blood sugar can lead to a range of health issues:
- Hypoglycemia: Low blood sugar can cause symptoms such as dizziness, irritability, and fatigue. If severe, it can lead to loss of consciousness.
- Hyperglycemia: High blood sugar, if persistent, can damage blood vessels and nerves, leading to complications like cardiovascular disease, kidney damage, and neuropathy.
- Insulin Resistance: When cells become less responsive to insulin, the body must produce more to achieve the same effect, increasing the risk of developing type 2 diabetes.
Women in perimenopause and menopause may experience greater challenges in blood sugar regulation due to hormonal fluctuations. Estrogen and progesterone influence insulin sensitivity, and as their levels decline, women may become more susceptible to blood sugar imbalances. This underscores the importance of monitoring blood sugar levels and adopting lifestyle changes to maintain balance during these life stages.
Menopause can be a stressful time, but managing stress is key to reducing symptoms like hot flashes and mood swings. Techniques such as deep breathing exercises, progressive muscle relaxation, and mindfulness meditation can be effective. Cognitive-behavioral therapy (CBT) has also been shown to improve psychological well-being. Engaging in hobbies, maintaining social connections, and seeking support from peers or professionals can further aid in managing stress during menopause.
The Critical Importance of Sleep
Sleep’s Role in Overall Health
Sleep is a fundamental human need, akin to breathing and eating. It is during sleep that the body and mind undergo restoration, healing, and strengthening. Quality sleep is associated with a myriad of health benefits, including improved cognitive function, emotional regulation, cardiovascular health, and immune system performance. Conversely, chronic sleep deprivation can lead to a host of health issues, such as obesity, diabetes, cardiovascular disease, and mental health disorders. For women in perimenopause and menopause, sleep becomes even more critical as their bodies navigate through hormonal changes that can be both physically and emotionally taxing.
Understanding Sleep Stages
Sleep is not a uniform state of rest but is composed of several stages that cycle throughout the night. These stages include non-REM (NREM) sleep, which has three phases, and REM (rapid eye movement) sleep. NREM sleep is the time when the body repairs tissues, builds bone and muscle, and strengthens the immune system. REM sleep, on the other hand, is when the brain processes information from the day, consolidates memories, and is also when most dreaming occurs. Each cycle of sleep stages lasts about 90 minutes, and a healthy night’s sleep will cycle through these stages multiple times.
Consequences of Sleep Deprivation
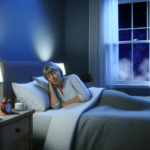
The consequences of insufficient sleep are far-reaching and can significantly impact a woman’s health during perimenopause and menopause. Sleep deprivation can exacerbate common menopausal symptoms such as hot flashes, mood swings, and cognitive disturbances. It can also lead to insulin resistance, which is particularly concerning as fluctuating and declining estrogen levels during menopause already increase the risk of metabolic syndrome and type 2 diabetes. Furthermore, poor sleep can lead to increased levels of the stress hormone cortisol, which can cause additional sleep disturbances and create a vicious cycle of sleeplessness and stress.
Given the profound impact of sleep on overall well-being, it is essential for women in perimenopause and menopause to prioritize sleep and adopt habits that promote restful nights. This includes establishing a regular sleep schedule, creating a comfortable sleep environment, and considering professional consultation if sleep disturbances persist.
Interconnection Between Sleep and Blood Sugar
How Blood Sugar Affects Sleep
Blood sugar levels have a profound impact on sleep quality and quantity. High blood sugar, or hyperglycemia, can lead to frequent urination throughout the night, disrupting sleep. This is due to the kidneys working to remove excess glucose from the bloodstream, which can also cause dehydration and the need to drink water, further interrupting sleep. Conversely, low blood sugar, or hypoglycemia, can trigger the release of stress hormones like adrenaline and cortisol, which may cause night sweats and nightmares, leading to abrupt awakenings. Thus, maintaining balanced blood sugar levels is crucial for uninterrupted, restful sleep.
Sleep Disturbances During Perimenopause and Menopause
During perimenopause and menopause, women often experience sleep disturbances. These can include difficulty falling asleep, staying asleep, and frequent awakenings during the night. Factors such as hormonal fluctuations, hot flashes, and night sweats contribute to these challenges. Additionally, the decline in estrogen and progesterone can disrupt the circadian rhythm, leading to insomnia and poor sleep quality. These sleep issues not only affect daytime energy and mood but can also exacerbate blood sugar dysregulation, creating a challenging cycle for women during this transitional phase.
The Bidirectional Relationship of Sleep and Blood Sugar
The relationship between sleep and blood sugar is bidirectional. Poor sleep can lead to increased insulin resistance, higher cortisol levels, and subsequent blood sugar imbalances. Elevated cortisol, particularly due to sleep deprivation, can increase glucose production in the liver, leading to higher blood sugar levels. On the other hand, unstable blood sugar levels can cause sleep disturbances. This interplay suggests that addressing one aspect can positively influence the other. Therefore, strategies to stabilize blood sugar may improve sleep, and enhancing sleep quality can help regulate blood sugar levels, highlighting the importance of a holistic approach to health during perimenopause and menopause.
Hormonal Changes and Their Impact on Blood Sugar and Sleep
Estrogen, Progesterone, and Blood Sugar Regulation
The hormonal fluctuations of perimenopause and menopause, particularly the decline in estrogen and progesterone, have a profound impact on blood sugar regulation. Estrogen influences the body’s sensitivity to insulin, the hormone responsible for facilitating glucose uptake into cells. As estrogen levels decrease, women may experience increased insulin resistance, leading to higher blood sugar levels. Progesterone, which also affects insulin sensitivity, sees a decline that can further exacerbate blood sugar imbalances. These hormonal changes can disrupt the delicate balance required for optimal blood sugar control, making it more challenging for women to maintain healthy glucose levels during perimenopause and menopause.
Insulin Resistance and Menopause
Insulin resistance is a condition where the body’s cells become less responsive to insulin, often leading to elevated blood sugar levels. During menopause, the drop in estrogen levels can contribute to the development of insulin resistance. This hormonal shift can cause the pancreas to work harder to produce more insulin in an attempt to lower blood sugar levels, which may eventually lead to type 2 diabetes if not managed properly. Women in menopause are at a higher risk of developing insulin resistance due to these hormonal changes, making it crucial to monitor blood sugar levels and adopt lifestyle changes that can improve insulin sensitivity.
The Role of Cortisol in Sleep and Blood Sugar
Cortisol, the body’s primary stress hormone, plays a significant role in regulating sleep and blood sugar. It follows a diurnal pattern, peaking in the early morning and declining throughout the day. During perimenopause and menopause, sleep disturbances can lead to elevated cortisol levels, which in turn can increase blood sugar by stimulating gluconeogenesis and reducing insulin sensitivity. High cortisol levels at night can interfere with sleep quality, creating a vicious cycle where poor sleep leads to higher cortisol levels, which then contribute to further sleep disruption and blood sugar dysregulation. Managing stress and improving sleep hygiene are essential strategies for breaking this cycle and supporting overall health during menopause.
Strategies for Managing Blood Sugar and Sleep
Lifestyle Changes for Blood Sugar Balance
Maintaining a balanced blood sugar level is crucial for overall health, especially during perimenopause and menopause. Lifestyle changes can significantly impact blood sugar regulation. Prioritizing consistent meal times can help stabilize blood sugar levels throughout the day. Additionally, incorporating regular physical activity into your routine can improve insulin sensitivity and aid in glucose management. It’s also important to focus on stress reduction techniques such as meditation, yoga, or deep breathing exercises, as stress can cause blood sugar levels to fluctuate.
Dietary Recommendations
A balanced diet plays a pivotal role in managing blood sugar. Emphasize a diet rich in fiber, whole grains, fruits, and vegetables, which can help slow the absorption of sugar into the bloodstream. Lean proteins and healthy fats are also essential, as they can contribute to satiety and further stabilize blood sugar levels. It’s advisable to limit the intake of processed foods, refined sugars, and high-glycemic carbohydrates to prevent spikes in blood sugar.
Exercise and Stress Management
Exercise is a powerful tool for managing blood sugar and stress. Engaging in both aerobic and anaerobic exercises can help the body’s sensitivity to insulin, which is often altered during menopause. Stress management is equally important, as elevated cortisol levels can lead to increased blood sugar. Practices such as mindfulness, guided imagery, and progressive muscle relaxation can mitigate stress and its effects on blood sugar and sleep.
Sleep Hygiene and Professional Consultation
Good sleep hygiene is essential for blood sugar control and overall health. Establishing a regular sleep schedule, creating a restful sleeping environment, and avoiding stimulants like caffeine close to bedtime can improve sleep quality. If sleep disturbances persist, it may be beneficial to seek a professional consultation. A healthcare provider can offer tailored advice and may suggest a sleep study to identify any underlying issues. In some cases, hormone therapy may be recommended to manage menopause symptoms that interfere with sleep.

Recommended by Health Care Professionals.
Loved by thousands of women who got their life back.
Conclusion: Integrating Self-Care for Better Health
Summarizing the Connection Between Hormones, Blood Sugar, and Sleep
The intricate dance between hormones, blood sugar, and sleep is a symphony that plays out within the female body, particularly during the transformative stages of perimenopause and menopause. Hormonal fluctuations characteristic of these phases can disrupt blood sugar regulation, leading to potential sleep disturbances. Conversely, poor sleep can exacerbate blood sugar imbalances, creating a cyclical challenge for women’s health. Estrogen and progesterone, key players in this scenario, not only influence reproductive functions but also have a profound impact on insulin sensitivity and glucose metabolism. As these hormones wane, women may experience increased insulin resistance and a higher propensity for sleep disorders, further complicating the management of blood sugar levels.
The Importance of Self-Care and Seeking Help
Self-care emerges as a pivotal strategy in navigating the complexities of hormonal changes, blood sugar regulation, and sleep quality. It encompasses a spectrum of actions, from adopting a balanced diet rich in fiber and low-glycemic foods to engaging in regular physical activity and stress reduction techniques. Women are encouraged to prioritize sleep hygiene, seek professional consultation when necessary, and consider the use of hormone replacement therapy under medical guidance. Embracing self-care is not merely about symptom management; it is about empowering women to take charge of their health and well-being during a time of significant transition.
Final Thoughts on Navigating Perimenopause and Menopause
As women journey through perimenopause and menopause, understanding the interplay between hormones, blood sugar, and sleep is crucial. By integrating self-care practices into daily life, women can mitigate the challenges posed by these changes. It is essential to recognize the value of professional support and the wealth of knowledge available from healthcare providers specializing in women’s health. With informed self-care, women can not only improve their quality of life during menopause but also lay the foundation for long-term health and vitality.