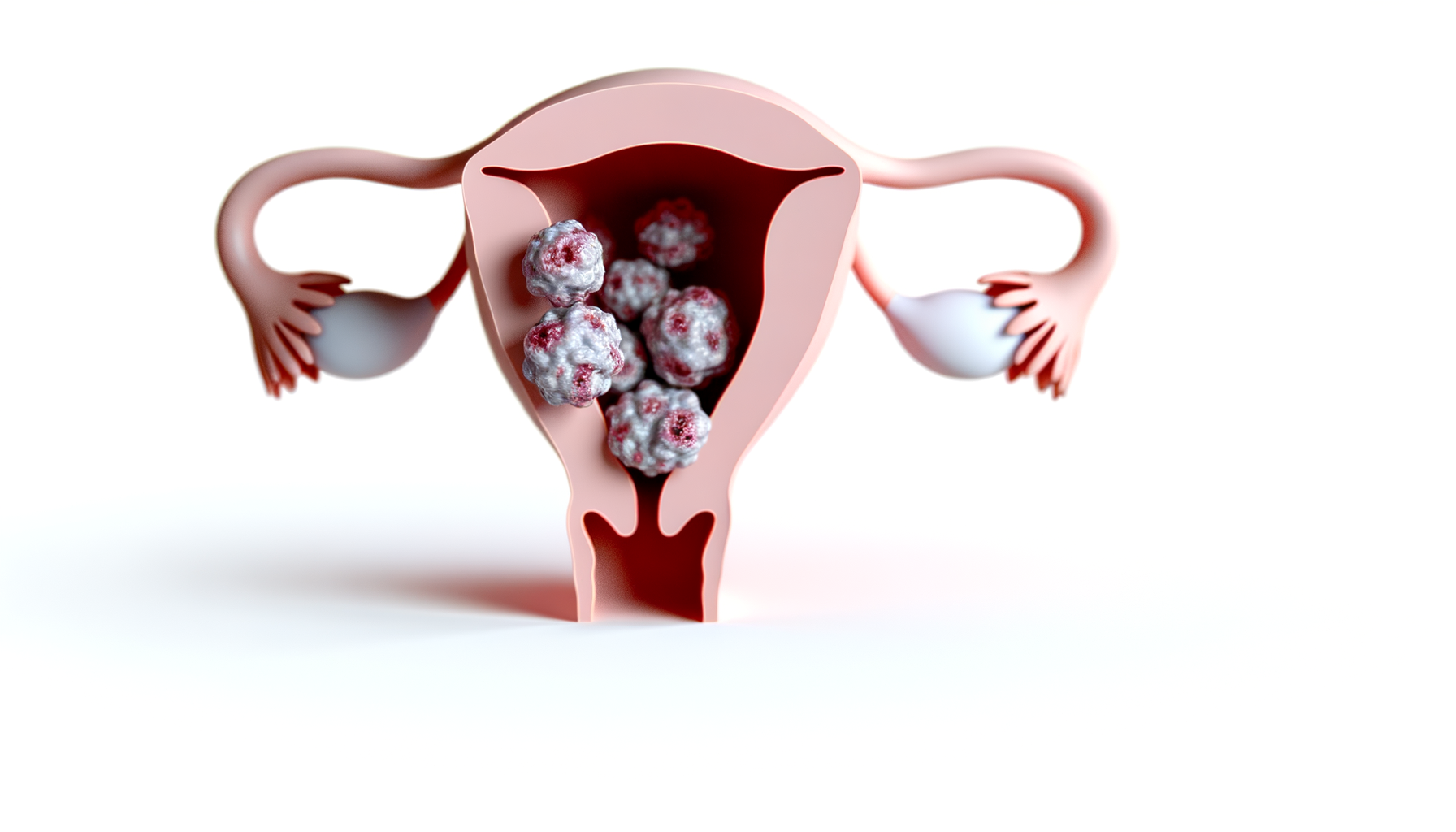
Uterine Polyps
Uterine polyps, also known as endometrial polyps, are benign (noncancerous) growths that appear on the inner lining of the uterus, an area called the endometrium. These polyps are typically soft and may be attached to the uterine wall by a large base or a thin stalk. Their sizes vary, ranging from as small as a sesame seed to as large as a golf ball or even bigger. A woman may have a single polyp or multiple polyps at once. While most uterine polyps are benign, they can cause symptoms that affect menstruation and fertility.
Prevalence and Demographics
Uterine polyps are more likely to develop during the perimenopausal period, typically in women in their 40s and 50s, and can also occur postmenopause. They are less common in women under 20 years of age. Factors such as obesity, hypertension, and the use of certain medications like tamoxifen, which is used to treat breast cancer, can increase the risk of developing uterine polyps. Genetic conditions such as Lynch syndrome or Cowden syndrome also heighten the risk. The exact prevalence of uterine polyps is challenging to determine since they often do not cause symptoms and therefore may go undiagnosed.
Types of Uterine Polyps
Uterine polyps can be classified based on their origin within the layers of the endometrium, their shape, and the presence of certain cell types. They may be sessile, with a broad base that directly attaches to the uterine wall, or pedunculated, hanging from a stalk. The composition of uterine polyps can vary, with some containing fibrous tissue, glands, blood vessels, or a combination of these elements.
Potential for Malignancy
Although the majority of uterine polyps are benign, there is a small risk that they can become cancerous, particularly in postmenopausal women. The transformation of a polyp into a malignancy is a concern, which necessitates careful monitoring and, in some cases, removal for histopathological examination. The risk of malignancy underscores the importance of regular medical checkups and appropriate diagnostic procedures for women with uterine polyps, especially for those with risk factors or who have undergone menopause.
Anatomy and Development
Cellular Origin and Growth
Uterine polyps, also known as endometrial polyps, are overgrowths of the endometrial tissue that lines the uterus. These polyps originate from the glandular epithelium and stroma of the endometrium and are thought to arise due to localized hyperplasia of these tissues. The exact pathogenesis of uterine polyps is not fully understood, but hormonal factors, particularly estrogen, play a significant role in their growth and development. The presence of a higher concentration of estrogen receptors within polyp glandular cells compared to the normal endometrium suggests a heightened sensitivity to estrogen stimulation, which may contribute to polyp growth.
Size and Shape Variations
Uterine polyps can vary greatly in size, ranging from a few millimeters to several centimeters, and can be as large as filling the entire uterine cavity. Their shape may also differ, with some polyps appearing as flat, sessile lesions with a broad base, while others are pedunculated, hanging from a thin stalk. The gross morphological appearance of these polyps is typically smooth, and they can be spherical or cylindrical in structure.
Attachment to the Uterine Wall
The attachment of uterine polyps to the uterine wall can be either broad-based (sessile) or on a narrow stalk (pedunculated). Sessile polyps are more closely integrated with the endometrial lining, while pedunculated polyps are attached by a thinner portion of tissue, which can sometimes extend into the cervical canal or even protrude into the vagina.
Polyp Multiplicity and Distribution
Uterine polyps can occur as solitary lesions or as multiple growths within the uterine cavity. They are most commonly found in the fundus and the cornual region of the uterus, which can present technical challenges for removal. The distribution of polyps is not uniform, and they may be more prevalent in certain areas of the endometrium. The multiplicity of polyps can have implications for symptoms, fertility, and the potential for malignancy.
In summary, the anatomy and development of uterine polyps involve a complex interplay of cellular growth, hormonal influences, and genetic factors. Understanding these aspects is crucial for the effective diagnosis and management of uterine polyps.

If you wonder, if this discomfort and the dryness down there will be there forever….
Try Mae. Mae is gives you back comfort, control, re-assurance, and re-connecting.
Mae is more than just a vaginal moisturizer; it’s your ally for intimate natural health, rediscovering joy, cultivating comfort, and even igniting sparks of intimacy and rekindled romance. Mae is your companion in rejoicing in your femininity at every stage of life. Learn more…
Symptoms of Uterine Polyps
Common Symptoms
Uterine polyps, or endometrial polyps, often present with a range of symptoms that can vary in intensity. The most frequent symptom associated with uterine polyps is irregular bleeding, which includes unpredictable vaginal spotting or bleeding between menstrual periods. Women may also experience heavy menstrual bleeding (menorrhagia), which can lead to anemia and fatigue. In some cases, bleeding may occur after menopause, which should always prompt medical evaluation. Additionally, polyps can sometimes prolapse through the cervix, causing discomfort and a sensation of pressure.
Asymptomatic Cases
It is not uncommon for uterine polyps to be asymptomatic, meaning they do not cause noticeable symptoms. This can make them difficult to detect without medical screening. Asymptomatic polyps are often discovered incidentally during routine examinations or imaging for other conditions. The absence of symptoms does not necessarily indicate that the polyps are harmless, as they can still impact overall uterine health and function.
Symptoms Indicative of Complications
While most uterine polyps are benign, certain symptoms may indicate potential complications or the presence of malignancy, especially in postmenopausal women. Postmenopausal bleeding is a particularly concerning symptom and warrants immediate medical attention. Other signs that could suggest complications include severe pain, which might indicate a twisted polyp stalk, or an infection if there is associated fever or foul-smelling discharge.
Impact on Fertility and Menstruation
Uterine polyps can have a significant impact on a woman’s reproductive health. They may interfere with fertility by obstructing the fallopian tubes or preventing a fertilized egg from implanting in the uterine lining. Polyps can also be a cause of miscarriage by creating an inhospitable environment for pregnancy. Regarding menstruation, polyps can lead to irregular menstrual cycles and unpredictable bleeding patterns, which can be distressing and disruptive to a woman’s daily life. Some studies suggest that polypectomy, the surgical removal of polyps, may improve fertility outcomes, although this is not universally guaranteed.
Causes and Risk Factors
Hormonal Factors
The development of uterine polyps is closely linked to hormonal fluctuations within the body, particularly the hormone estrogen. Estrogen is responsible for the thickening of the endometrial lining each menstrual cycle, and an overgrowth of this lining can lead to the formation of polyps. Women experiencing changes in estrogen levels, such as those approaching or undergoing menopause, are at a heightened risk of developing uterine polyps.
Genetic Predispositions
Genetic factors may also play a role in the development of uterine polyps. Individuals with certain hereditary conditions, such as Lynch syndrome or Cowden syndrome, are at an increased risk. These genetic syndromes can predispose a person to a variety of health issues, including a higher likelihood of developing uterine polyps.
Lifestyle and Environmental Influences
Lifestyle choices and environmental factors can contribute to the risk of developing uterine polyps. Obesity, characterized by a Body Mass Index (BMI) of 30 or higher, has been associated with an increased risk of polyp formation. High blood pressure, or hypertension, is another condition that can elevate the risk. Additionally, the use of certain medications, such as tamoxifen for breast cancer treatment, and hormone replacement therapies that involve high doses of estrogen, have been linked to the development of uterine polyps.
Age and Menopausal Status
Age is a significant risk factor for uterine polyps. Women in their 40s and 50s, particularly those who are perimenopausal or postmenopausal, are more likely to develop polyps. This increased risk is thought to be due to the hormonal changes that occur during this stage of a woman’s life. As estrogen levels fluctuate and eventually decline, the endometrium can respond in ways that promote polyp growth.
In conclusion, while the exact cause of uterine polyps is not fully understood, a combination of hormonal factors, genetic predispositions, lifestyle influences, and age-related changes are all recognized as contributing to the risk of developing these growths. Understanding these risk factors can help in early detection and management of uterine polyps.

THEN IT CONTAINS TOXIC CHEMICALS. WHY RISK IT GETTING SICK? GO CHEMICAL FREE.
Diagnosis of Uterine Polyps
Initial Examination and Patient History
The diagnostic process for uterine polyps typically begins with a thorough initial examination and review of the patient’s medical history. During the initial consultation, healthcare providers will inquire about symptoms such as irregular menstrual bleeding, spotting between periods, or bleeding after menopause. They will also ask about any history of hormone therapy, medications like tamoxifen, and any family history of hereditary conditions like Lynch syndrome or Cowden syndrome that may increase the risk of polyps. A physical examination, including a pelvic exam, may provide the first indication of the presence of uterine polyps.
Imaging and Diagnostic Tests
Following the initial assessment, various imaging and diagnostic tests are employed to visualize the interior of the uterus and confirm the presence of polyps. The most common imaging test is a transvaginal ultrasound, where a wand-like device is inserted into the vagina to create images of the uterus using sound waves. For a more detailed view, a hysterosonography or sonohysterography may be performed, which involves the insertion of saline solution into the uterus via a catheter during the ultrasound to expand the uterine cavity and provide clearer images.
In some cases, a hysteroscopy is conducted, which involves inserting a thin, flexible, lighted telescope called a hysteroscope through the vagina and cervix into the uterus. This allows the doctor to directly observe the uterine lining and polyps. If polyps are identified, they can often be removed during the same procedure.
Biopsy and Histopathological Analysis
To determine the nature of the polyps, a biopsy may be performed. This involves the collection of a tissue sample from the polyp using a soft plastic tool or a curette in a procedure known as curettage. The tissue sample is then sent to a laboratory for histopathological analysis to check for cancer cells and to provide a definitive diagnosis.
Differential Diagnosis
It is important to distinguish uterine polyps from other conditions that can cause similar symptoms, such as fibroids, which are overgrowths of the muscle inside the walls of the uterus. This process, known as differential diagnosis, ensures that the appropriate treatment is provided. While the same tests can detect both fibroids and polyps, the hysteroscopy allows the doctor to visually differentiate between the two based on their appearance and location within the uterus.
Overall, the diagnosis of uterine polyps involves a combination of clinical evaluation, imaging studies, and tissue sampling to accurately identify and assess the polyps. This comprehensive approach is crucial for determining the appropriate management and treatment strategies for each individual patient.
By the way, something for you, a little gift!!!
I am just in the middle of publishing my book. It’s about How women can balance their hormones. One part is about food and diet, of course.
Follow this link and enter your email.
I will send you this part of the book for free once the book is published. It has many concrete, practical tips and recipes and will help you feel better during menopause or times of Big hormonal fluctuations.
Annette, Damiva Lead for Health & Wellness

Treatment Options
Watchful Waiting and Non-Invasive Approaches
For individuals with uterine polyps that are asymptomatic and show no signs of malignancy, a conservative approach known as watchful waiting may be recommended. This involves regular monitoring without immediate intervention, as some polyps may regress on their own, particularly in premenopausal women. During this period, patients are advised to stay vigilant for any new or worsening symptoms and to maintain regular follow-up appointments with their healthcare provider.
Medications and Hormonal Treatments
When symptoms are present, or if there is a need to manage the polyps non-surgically, medications and hormonal treatments may be utilized. Progestins and gonadotropin-releasing hormone (GnRH) agonists are commonly prescribed to help control hormone levels, potentially shrinking the polyps and alleviating symptoms such as heavy menstrual bleeding. However, it is important to note that the relief provided by these medications is often temporary, and symptoms may return once the medication is discontinued.
Surgical Interventions
In cases where polyps are symptomatic, large, or there is a suspicion of cancer, surgical interventions are considered. The most common procedure for removing uterine polyps is a hysteroscopy, where a thin, lighted instrument is inserted through the vagina and cervix to access and remove the polyps. Another method is curettage, which involves scraping the uterine lining to remove polyps. For polyps with cancerous cells or significant risk factors for uterine cancer, a more extensive surgery, such as a hysterectomy (removal of the uterus), may be necessary.
Post-Treatment Monitoring and Recurrence Prevention
Following treatment, post-treatment monitoring is crucial to ensure the complete removal of polyps and to check for signs of recurrence. Regular follow-up visits, which may include imaging tests or hysteroscopy, help in early detection and management of any new polyps. To prevent recurrence, patients may be advised to manage risk factors such as maintaining a healthy weight and blood pressure. Additionally, hormone therapy may be adjusted to reduce the likelihood of polyp regrowth.
While there is no guaranteed method to prevent uterine polyps, adopting a healthy lifestyle and adhering to recommended follow-up care can significantly contribute to the overall well-being of individuals affected by this condition.
Conclusion and Future Directions
Summary of Key Points
Uterine polyps are benign growths that arise from the endometrial lining of the uterus, presenting a range of symptoms from abnormal bleeding to asymptomatic cases. While the majority of polyps do not pose a significant risk for malignancy, their presence can impact fertility and menstruation. The development of polyps is influenced by hormonal imbalances, particularly an excess of estrogen, and can be exacerbated by factors such as obesity, age, and genetic predispositions. Diagnosis typically involves imaging techniques like transvaginal ultrasound and hysteroscopy, often complemented by biopsy for histopathological analysis. Treatment options range from watchful waiting to surgical interventions, with the choice of treatment depending on the individual’s symptoms, risk factors, and reproductive goals.
Advancements in Research and Treatment
Recent research has focused on understanding the cellular mechanisms behind polyp formation and recurrence, leading to improved diagnostic and treatment methods. Advancements in imaging technology have enhanced the detection of polyps, while hysteroscopic techniques have refined the precision of polyp removal. Studies continue to explore the role of hormonal management in preventing polyp regrowth, with an emphasis on personalized medical approaches that consider the patient’s hormonal profile and risk factors.
Recommendations for Affected Individuals
- Regular Monitoring: Individuals with a history of uterine polyps should undergo regular follow-up exams to detect any recurrence early.
- Lifestyle Modifications: Maintaining a healthy weight and balanced diet may help reduce the risk of polyp development and recurrence.
- Informed Decision-Making: Discuss all available treatment options with a healthcare provider to make informed decisions that align with personal health goals.
- Understanding Risks: Be aware of the potential for malignancy, although rare, and the implications of polyps on fertility and menstrual health.
Thus, uterine polyps are a common gynecological condition that can have significant implications for women’s reproductive health. While the prognosis is generally good, with most polyps being benign and treatable, the potential for recurrence and impact on fertility necessitates ongoing vigilance and management. Future research promises to unveil deeper insights into the etiology of polyps, leading to more targeted and effective treatments. As we advance our understanding of these pesky polyps, the goal remains to provide comprehensive care that empowers women to lead healthy lives, free from the burden of uterine polyps.