Understanding Perimenopause
Perimenopause is the phase of a woman’s life leading up to menopause, the point at which she no longer experiences menstrual periods. This transitional period is characterized by fluctuations in a woman’s menstrual cycle and can begin several years before menopause. Most women enter perimenopause in their 40s, but it can start as early as the 30s or as late as the 50s. The duration of perimenopause varies, typically lasting between 4 and 8 years, until a woman has gone 12 consecutive months without a menstrual period, signifying the onset of menopause.
Hormonal Changes and Their Effects
During perimenopause, the ovaries gradually produce less estrogen, leading to changes in the menstrual cycle and other physical and emotional symptoms. These hormonal fluctuations can cause irregular periods, heavy bleeding, and cramping. High levels of estrogen can lead to symptoms such as bloating, breast tenderness, and heavier menstrual bleeding, while low levels can result in vaginal dryness, insomnia, and hot flashes. The hormonal changes are also responsible for the decrease in fertility during this time.
Duration and Transition to Menopause
The perimenopausal phase can last anywhere from 2 to 10 years. As a woman approaches the end of perimenopause, estrogen levels drop significantly, leading to fewer and eventually the cessation of menstrual periods. This transition to menopause is a natural biological process, but the symptoms can be managed with lifestyle changes, home remedies, and medical treatments to ease the discomfort associated with this stage of life.
Testosterone Levels and Age Correlation
While estrogen and progesterone are the primary hormones discussed in relation to perimenopause, testosterone levels also play a role in a woman’s health. Testosterone levels in women typically begin to decline in their 30s and continue to decrease, reaching about half their peak levels by the time of menopause. This decline in testosterone is more closely related to aging than to the hormonal changes of perimenopause or menopause itself. However, it can still contribute to changes in mood, sexual desire, and energy levels.
Symptoms of Perimenopause
Menstrual Cycle Irregularities
One of the hallmark signs of perimenopause is the change in the menstrual cycle. As women approach menopause, their menstrual periods can become irregular. This may manifest as changes in the timing, frequency, duration, and flow of periods. Some women may experience shorter cycles, while others may have longer ones. It is also common for periods to be skipped altogether. In the later stages of perimenopause, women may start missing periods for several months at a time. These irregularities are primarily due to the fluctuating levels of estrogen and progesterone as the ovaries gradually reduce hormone production.
Physical Symptoms Linked to Hormone Levels
The physical symptoms experienced during perimenopause are directly linked to the changing hormone levels in a woman’s body. High levels of estrogen can lead to symptoms such as:
- Bloating
- Cramping
- Heavier than normal bleeding
- Breast tenderness
Conversely, low levels of estrogen can cause:
- Vaginal dryness
- Insomnia
- Hot flashes and night sweats
- Headaches
- Unexplained exhaustion
- Osteoporosis or loss of bone density
Changes in progesterone levels can result in:
- Heavier and longer menstruation
- Irregular menstruation
These hormonal fluctuations can also lead to increased menstrual cramping and discomfort, often requiring management through lifestyle changes or medical intervention.
Psychological and Mood Changes
Perimenopause can also bring about psychological and mood changes. Many women report experiencing mood swings, irritability, anxiety, and even depression during this transitional phase. The exact relationship between these mood changes and hormonal fluctuations is complex and not fully understood. However, it is clear that the ups and downs of estrogen and progesterone can significantly impact brain chemistry and, consequently, mood and emotional well-being.
Women who have a history of depression or are under significant stress may be more susceptible to these mood changes. It is important for women to monitor their mental health during perimenopause and seek support or treatment if needed. Lifestyle modifications, such as regular exercise and stress management techniques, can be beneficial in managing psychological symptoms. In some cases, healthcare providers may recommend therapy or medication to help stabilize mood during this period.
Overall, the symptoms of perimenopause can vary widely from one individual to another. While some women may navigate this transition with minimal discomfort, others may find the symptoms more challenging. Understanding these changes and seeking appropriate care can help manage perimenopausal symptoms effectively.
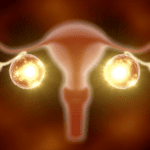
Ovary Pain During Perimenopause
Causes of Ovary Pain
Ovary pain during perimenopause can be a distressing symptom for many women. It is often felt in the lower abdomen and pelvis, and sometimes even in the lower back. The pain may be persistent, come and go, be dull, or progress to sharp bursts of pain. There are several conditions related to the reproductive system that can cause ovary pain during this transitional phase:
- Ovulation: Ovulation pain, also known as mittelschmerz, can occur mid-cycle and vary in intensity.
- Menstrual Pain: Dysmenorrhea may worsen during perimenopause due to hormonal changes.
- Endometriosis: This condition involves endometrial tissue growing outside the uterus, causing severe cramping and heavy menstrual flow.
- Uterine Fibroids: Noncancerous tumors in the uterus that may cause heavy bleeding and worse cramping.
- Ovarian Cysts: Fluid-filled masses on the ovaries that can cause pain, especially if they rupture or cause ovarian torsion.
- Pelvic Inflammatory Disease (PID): An infection in the reproductive organs that can cause lower abdominal or pelvic pain.
- Ovarian Cancer: Although rare, ovarian cancer can cause persistent and severe pain.
- Polycystic Ovary Syndrome (PCOS): A hormonal disorder causing irregular periods, weight gain, and ovarian cysts.
It’s also possible to have lower abdominal pain that does not come from the reproductive system, such as appendicitis, which can be life-threatening.
When to Seek Medical Attention
Women should be vigilant about their health and seek medical attention if they experience severe, chronic, or unexplainable abdominal pain. It is particularly important to consult a healthcare provider if:
- The pain is new, has changed, or is getting worse.
- Menstrual flow is heavier than usual or period pain worsens and does not improve with treatment.
- There is vaginal bleeding after menopause.
- Pelvic pain disrupts daily life or worsens during or after sexual activity.
Emergency medical attention is necessary when sharp pelvic pain is accompanied by symptoms such as vaginal bleeding, blood in the urine, nausea or vomiting, dizziness or fainting, low blood pressure, shoulder pain, rectal pressure, fever, or if pregnant or using an intrauterine device (IUD).
Diagnosing the cause of ovary pain may involve a combination of self-checks, history and physical examination, labs and tests, and imaging. It is essential to rule out other causes of pain and to identify the correct diagnosis to receive appropriate treatment.
Understanding the causes and knowing when to seek medical help can empower women to manage their health effectively during perimenopause. It is crucial to listen to one’s body and not dismiss persistent or severe ovary pain as a normal part of the transition.
Managing Symptoms at Home
Home Remedies for Cramping
Perimenopause can bring about a variety of symptoms, including increased cramping during menstrual periods. Fortunately, there are several home remedies that can help alleviate this discomfort:
- Heat Therapy: Applying a heating pad, hot water bottle, or warm cloth to your abdomen can help relax the muscles and reduce cramps. The warmth provides a soothing effect that can offer immediate relief.
- Warm Baths: Soaking in a warm bath can also ease cramps by increasing blood flow and relaxing the pelvic muscles.
- Gentle Exercise: Activities such as walking, yoga, or stretching can improve circulation and help reduce the intensity of cramps.
- Hydration: Drinking plenty of water can prevent dehydration, which may worsen muscle cramps.
- Abdominal Massage: Gently massaging your lower abdomen can help to relieve tension and cramping. Using essential oils like lavender or peppermint may enhance the relaxing effects.
- Stress Reduction Techniques: Stress can exacerbate cramps, so practices like deep breathing, meditation, or other relaxation techniques can be beneficial.
Lifestyle Adjustments
Making certain lifestyle adjustments can also play a significant role in managing perimenopausal symptoms:
- Diet: Eating a balanced diet rich in fiber, omega-3 fatty acids, and essential nutrients can help regulate hormonal fluctuations. Limiting intake of caffeine, alcohol, and high-sodium foods may also reduce bloating and cramps.
- Regular Exercise: Maintaining a regular exercise routine can improve overall health and help manage symptoms. Exercise can also help stabilize mood and improve sleep quality, which can be disrupted during perimenopause.
- Sleep Hygiene: Establishing a regular sleep schedule and creating a restful environment can help combat insomnia and fatigue associated with perimenopause.
- Smoking Cessation: If you smoke, consider quitting. Smoking can worsen perimenopausal symptoms and increase the risk of developing other health issues.
- Stress Management: Chronic stress can aggravate symptoms, so finding effective ways to manage stress is crucial. Techniques may include time management strategies, seeking social support, and engaging in hobbies or activities that you enjoy.
While these home remedies and lifestyle adjustments can be effective for managing symptoms, it’s important to consult with a healthcare provider if symptoms persist or worsen. They can provide guidance and additional treatment options tailored to your specific needs.

Medical Treatments and Interventions
Over-the-Counter Medications
For many women navigating the perimenopausal phase, over-the-counter (OTC) medications can be a first line of defense against the discomfort associated with hormonal fluctuations. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, are commonly used to alleviate cramping and pain. These medications work by reducing the production of prostaglandins, which are compounds associated with inflammation and pain. For those who prefer an alternative to NSAIDs, acetaminophen can be effective in managing pain, though it does not have the anti-inflammatory properties of NSAIDs.
Additionally, some women find relief using analgesic transdermal patches or gels containing ingredients like camphor, menthol, capsaicin, or methyl salicylate. These topical treatments provide localized pain relief and can be particularly useful for managing lower abdominal and pelvic discomfort. It is important to follow the recommended dosages and to be aware of any potential side effects, such as gastrointestinal issues with NSAIDs or liver damage with excessive acetaminophen use.
Prescription Options
When OTC medications are insufficient in managing perimenopausal symptoms, prescription options may be considered. Hormone therapy, using estrogen or a combination of estrogen and progestins, can help stabilize hormone levels and alleviate symptoms such as heavy bleeding and severe cramping. However, hormone therapy is not suitable for everyone and should be discussed with a healthcare provider, considering the individual’s medical history and risk factors.
For women experiencing severe cramping that disrupts daily life, a low-dose birth control pill, patch, ring, or intrauterine device (IUD) may be prescribed. These methods can help regulate menstrual cycles, reduce the heaviness of periods, and provide more predictable symptom management. In cases where pain is particularly debilitating, a healthcare provider may prescribe stronger pain medications, though these are typically used sparingly due to the risk of dependency and other side effects.
Antidepressants may also be prescribed to help stabilize mood swings and assist with psychological symptoms associated with perimenopause. It is crucial for women to have open and ongoing discussions with their healthcare providers about the benefits and risks of any prescription medication, as well as any changes in their symptoms or overall health.
In conclusion, the management of perimenopausal symptoms, including ovary pain, involves a combination of self-care, OTC medications, and possibly prescription treatments. Women should work closely with their healthcare providers to determine the most appropriate and effective treatment plan for their individual needs.
Dietary and Lifestyle Changes
Nutrition and Hydration
During perimenopause, the body undergoes significant hormonal changes that can affect overall well-being. Nutrition plays a crucial role in managing these changes. A balanced diet rich in a variety of nutrients can help stabilize mood swings, improve energy levels, and mitigate some physical symptoms associated with perimenopause.
Key dietary recommendations include:
- High-fiber foods: Incorporate whole grains, beans, nuts, seeds, fruits, and vegetables to help with digestion and the elimination of excess hormones.
- Phytoestrogens: Foods such as soybeans, flaxseeds, and sesame seeds contain plant-based estrogens that may help balance fluctuating hormone levels.
- Calcium and Vitamin D: These nutrients are vital for bone health, which can be compromised due to hormonal changes. Dairy products, leafy greens, and fortified foods are good sources.
- Omega-3 fatty acids: Found in fatty fish, walnuts, and flaxseeds, omega-3s can help reduce inflammation and may alleviate mood swings.
- Water: Staying well-hydrated is essential for overall health and can help reduce bloating and improve skin elasticity.
It’s also advisable to limit intake of caffeine, alcohol, and high-sodium foods, as these can exacerbate symptoms like hot flashes, night sweats, and bloating.
Exercise and Stress Management
Regular physical activity and stress management are two pillars of a healthy lifestyle, especially during perimenopause. Exercise can help alleviate symptoms such as weight gain, mood swings, and sleep disturbances. It also promotes cardiovascular health and bone density, reducing the risk of osteoporosis.
Effective forms of exercise include:
- Aerobic activities: Brisk walking, cycling, and swimming can help maintain a healthy weight and improve cardiovascular health.
- Strength training: Weight-bearing exercises are crucial for bone health and maintaining muscle mass.
- Flexibility and balance: Yoga and Pilates can improve flexibility, reduce stress, and enhance mental well-being.
Stress management is equally important, as stress can exacerbate perimenopausal symptoms. Techniques such as deep breathing, meditation, and mindfulness can help manage stress levels. Additionally, ensuring adequate sleep and engaging in hobbies or activities that bring joy can contribute to a more balanced and fulfilling lifestyle.
In conclusion, dietary and lifestyle changes can have a profound impact on managing perimenopausal symptoms. A focus on nutrition and hydration, combined with regular exercise and stress management, can help navigate this transitional phase with greater ease and comfort.

Bette 100% All-Natural Relaxing Lavender Body Lotion.
Chemical-Free
Your relaxing night time body moisturizer to leave the day’s stress behind. Decompress and wish your body good night with the calming scent of lavender.
Alternative Therapies and Supplements
Complementary Practices
Many women seek out complementary practices as a way to manage perimenopause symptoms, including ovary pain. These practices often focus on holistic well-being and can include:
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body to balance energy flow. Some women find it helpful for reducing pain and stress.
- Yoga and Tai Chi: These gentle forms of exercise emphasize breathing, stretching, and flowing movements, which can improve flexibility, reduce stress, and potentially alleviate cramps and pain.
- Meditation and Mindfulness: Regular meditation can help manage stress, which may in turn reduce the severity of perimenopause symptoms.
- Massage Therapy: Massage can relax tense muscles, improve circulation, and provide relief from pain and discomfort.
Herbal and Vitamin Supplements
Some women find relief from perimenopause symptoms through herbal and vitamin supplements. Common supplements include:
- Black Cohosh: Often used for hot flashes and mood swings, it may also help with menstrual irregularities and pain.
- Vitamin D and Calcium: Essential for bone health, especially important as estrogen levels decline.
- Omega-3 Fatty Acids: Found in fish oil and flaxseed, they can help reduce inflammation and may alleviate cramps.
- Vitamin E: Some women report reduced hot flashes with vitamin E.
- Phytoestrogens: Found in soy and other plants, these compounds mimic estrogen and may provide some symptom relief.
- Magnesium: This mineral can help with sleep issues and muscle relaxation, potentially easing cramps.
It’s important to note that the effectiveness of these supplements can vary, and some may interact with other medications.
Precautions and Consultation with Healthcare Providers
Before starting any alternative therapy or supplement, it’s crucial to:
- Consult with a Healthcare Provider: Discuss any new treatments with your doctor, especially if you have underlying health conditions or are taking other medications.
- Research Quality: Choose high-quality supplements from reputable sources to avoid contaminants and ensure potency.
- Monitor for Side Effects: Be aware of any changes in your health and report adverse effects to your healthcare provider immediately.
- Understand Interactions: Some supplements can interfere with prescription medications or have contraindications with certain health conditions.
Ultimately, while alternative therapies and supplements can be part of a comprehensive approach to managing perimenopause symptoms, they should be used thoughtfully and in coordination with professional medical advice.