Understanding Menopause: Age Range and Symptoms
Menopause marks a significant transition in a woman’s life, typically occurring between the ages of 45 and 55, with an average onset at 51 years. It signifies the end of menstrual cycles and reproductive fertility. Symptoms vary widely among women but commonly include hot flashes, night sweats, vaginal dryness, and mood changes. These symptoms result from the decline in estrogen and progesterone production by the ovaries. The perimenopausal phase, which precedes menopause, can bring about irregular periods and hormonal fluctuations, often beginning several years before menopause itself.
Health Risks Associated with Menopause
With the onset of menopause, women face an increased risk of various health conditions. The decline in estrogen levels is associated with osteoporosis, a condition characterized by weakened bones and an elevated risk of fractures. Cardiovascular disease risk also rises post-menopause, as estrogen’s protective effects on heart and artery health diminish. Additionally, menopause can lead to an increased risk of certain cancers, such as breast and ovarian cancer, and exacerbate urogenital symptoms, impacting quality of life.
Overview of Menopause Screening Benefits
Menopause screening offers numerous benefits, including early detection of osteoporosis, allowing for timely intervention to prevent fractures. Screening can also aid in the identification of cardiovascular risks, guiding lifestyle modifications and treatments to mitigate heart disease. Furthermore, it can lead to the early detection of menopause-related cancers, improving outcomes through early treatment. Regular health assessments during and after the menopausal transition enable healthcare providers to develop personalized treatment plans that address individual symptoms and risks. Ultimately, menopause screening contributes to monitoring overall health and implementing preventive care strategies, providing mental well-being and peace of mind for women navigating this stage of life.
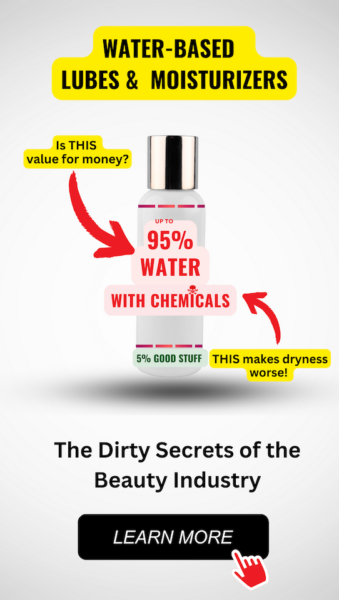
Feeling You Have a Right to Safe Beauty & Fem Care?
If so, it may be time for a change. It starts with knowledge. We have a few suggestions in our new guides.
Comprehensive Benefits of Menopause Screening
Early Detection of Osteoporosis and Heart Disease
Menopause screening plays a pivotal role in the early detection of osteoporosis, a condition where bones become brittle and fragile from loss of tissue. This is often due to hormonal changes, or deficiency of calcium or vitamin D. Screening can identify women at risk, allowing for preventive measures such as lifestyle changes and medication to strengthen bone density. Similarly, heart disease risk increases after menopause due to changes in estrogen levels affecting cholesterol and blood vessels. Through screening, healthcare providers can assess risk factors like blood pressure and lipid levels, enabling early intervention to prevent cardiovascular complications.
Identification of Menopause-Related Cancers
Menopause screening is essential for the identification of cancers that have an increased risk of developing during and after the menopausal transition, such as breast, ovarian, and endometrial cancers. Regular mammograms, pelvic exams, and Pap tests can lead to the detection of cancers at an early, more treatable stage. This proactive approach can significantly improve survival rates and reduce the need for aggressive treatments.
Development of Personalized Treatment Plans
Each woman experiences menopause differently, with a variety of symptoms and risk factors. Menopause screening allows healthcare providers to develop personalized treatment plans tailored to the individual’s needs. This may include hormone replacement therapy, lifestyle modifications, or other interventions to manage symptoms and reduce the risk of chronic conditions associated with menopause.
Monitoring Overall Health and Preventive Care
Menopause screening is not just about reproductive health; it’s a comprehensive review of a woman’s overall health. It includes assessments of bone density, cardiovascular health, and screening for diabetes and thyroid disorders. This holistic approach ensures that women receive preventive care to maintain their health and quality of life during the postmenopausal years.
Mental Well-being and Peace of Mind
The transition into menopause can be a source of anxiety for many women. Screening provides mental well-being by offering reassurance and peace of mind through knowledge and understanding of their health status. It also opens up opportunities for women to discuss their concerns with healthcare providers and receive support and counseling if needed.
Thus, menopause screening is a critical component of women’s healthcare that offers numerous benefits, including the prevention and early detection of diseases, personalized care, and the promotion of mental well-being. By embracing regular screening, women can take charge of their health during menopause and beyond.
Common chemicals can hurt your gut health, your skin health, your mental health, and immune system.
Do you know the three main ways that your body gets in touch with harmful chemicals?
Knowledge is Power!
The Ultimate Detox Guide will tell you how to lower your exposure to harmful chemicals!
Preparing for Menopause Screening
Consulting with Healthcare Providers
Before embarking on menopause screening, it is crucial to consult with healthcare providers who are knowledgeable about menopausal health. This initial consultation should include a discussion about your current symptoms, medical history, and any concerns you may have about entering menopause. Your healthcare provider can offer guidance on the types of screenings that are appropriate for your age and health status, as well as address any questions about the screening process. It is also an opportunity to discuss the potential need for hormone level tests, such as follicle-stimulating hormone (FSH) and estrogen (estradiol), or thyroid function tests, which can be influenced by menopause.
Understanding Individual Risk Factors
Each woman’s experience with menopause is unique, and understanding your individual risk factors is essential for effective screening. Risk factors can include age, family history of osteoporosis, cardiovascular disease, or specific cancers, as well as personal medical history such as previous surgeries or chronic conditions. Lifestyle factors, such as diet, exercise habits, and tobacco or alcohol use, also play a significant role in menopausal health. By evaluating these risk factors, healthcare providers can tailor screening recommendations to your specific needs, potentially including additional tests or more frequent monitoring for certain conditions.
Scheduling Appropriate Screenings
Once you have consulted with your healthcare provider and understood your individual risk factors, the next step is to schedule the appropriate screenings. These may include a bone density test to assess for osteoporosis, mammograms for breast cancer detection, Pap tests for cervical cancer screening, and lipid panels for heart disease risk assessment. The timing and frequency of these screenings will depend on your age, health history, and the presence of any symptoms or risk factors. It is important to adhere to the recommended screening intervals to ensure that any health issues are detected early and managed effectively.
Remember, menopause screening is not just about detecting health problems; it’s also an opportunity for preventive care. By taking proactive steps and partnering with healthcare providers, you can navigate the menopausal transition with confidence and maintain your health and well-being.
Key Menopause Screenings Explained
Bone Density Test for Osteoporosis
Osteoporosis is a significant health risk for postmenopausal women due to the steep increase in osteoporosis risk with estrogen withdrawal at menopause. A bone density test, commonly known as a dual-energy x-ray absorptiometry (DEXA), is a critical screening tool that measures bone mineral density (BMD). This test can detect osteoporosis before a fracture occurs and predict one’s chances of fracturing in the future. It is recommended for women at menopause and particularly for those with risk factors such as a family history of osteoporosis, previous fractures, or long-term use of medications that can weaken bones.
Mammogram for Breast Cancer Detection
A mammogram is an x-ray of the breast and is the most effective method for early detection of breast cancer. Regular mammograms can help find cancer at an early stage when treatment is most successful. The U.S. Preventive Services Task Force (USPSTF) recommends that women aged 50 to 74 years have a mammogram every two years. Women who are at higher risk may need to start screening earlier and may benefit from more frequent screenings.
Pap Test for Cervical Cancer Screening
The Pap test, also known as a Pap smear, checks for changes in the cells of the cervix that could lead to cervical cancer. This test can also detect infections and abnormalities. It is recommended that women begin cervical cancer screening at age 21 and continue until age 65, with the frequency depending on age and health history. Women over 30 may also have the option of co-testing with a human papillomavirus (HPV) test.
Lipid Panel for Heart Disease Risk Assessment
Cardiovascular disease is a leading cause of death in postmenopausal women. A lipid panel is a blood test that measures levels of cholesterol and triglycerides, which are indicators of heart disease risk. High levels of low-density lipoprotein (LDL) cholesterol and triglycerides, along with low levels of high-density lipoprotein (HDL) cholesterol, can increase the risk of heart disease and stroke. Screening recommendations vary, but adults should generally have their cholesterol checked every 4 to 6 years.
These screenings are vital components of preventive healthcare for postmenopausal women. By detecting potential health issues early, women can work with their healthcare providers to manage risks and maintain their health and well-being during the postmenopausal years.
By the way, something for you, a little gift!!!
I am just in the middle of publishing my book. It’s about How women can balance their hormones. One part is about food and diet, of course.
Follow this link and enter your email.
I will send you this part of the book for free once the book is published. It has many concrete, practical tips and recipes and will help you feel better during menopause or times of Big hormonal fluctuations.
Annette, Damiva Lead for Health & Wellness

Frequency and Timing of Menopause Screenings
Personalizing Screening Intervals
Menopause screening is not a one-size-fits-all approach. The frequency and timing of screenings should be personalized based on a woman’s individual health status, symptoms, and risk factors. While some women may require more frequent monitoring, others may need less. Personalizing screening intervals ensures that each woman receives the appropriate level of care and attention to her specific needs during the menopausal transition.
Age-Specific Recommendations
Generally, menopause screening should begin for most women around the age of 45 to 50. This is the average age range when menopausal symptoms typically start to appear. However, for women who experience early menopause or premature ovarian failure, screenings may need to start earlier. Age-specific recommendations help in identifying menopause-related health risks at the right time, allowing for timely interventions.
Adjusting for Health and Family History
Women with a family history of osteoporosis, heart disease, or menopause-related cancers may require earlier and more frequent screenings. Additionally, those with pre-existing health conditions such as diabetes or hypertension may also need tailored screening schedules. Adjusting the frequency and timing of menopause screenings based on health and family history helps in early detection and prevention of potential complications.
It is essential for healthcare providers to work closely with their patients to determine the most suitable screening schedule. Regular assessments and open communication about any changes in symptoms or health status are crucial for adjusting screening intervals as needed. By doing so, women can receive the most effective care throughout their menopausal years.
Challenges and Considerations in Menopause Screening
Addressing Barriers to Access
Access to menopause screening can be hindered by a variety of factors, including geographical location, lack of awareness, and socio-economic constraints. To improve access, it is essential to increase public education on the importance of menopause screening. Community outreach programs and mobile clinics can help reach women in remote areas. Additionally, healthcare providers should be trained to recognize menopausal symptoms and the need for screening, ensuring that women receive appropriate referrals and support.
Navigating Insurance and Costs
The cost of menopause screening and related treatments can be a significant barrier for many women. Insurance coverage for screenings varies widely, and out-of-pocket expenses can be prohibitive. Women should be encouraged to understand their insurance benefits and advocate for coverage of essential screenings. Healthcare providers can assist by providing clear information on the costs of various screening options and by supporting patients in navigating insurance claims and exploring financial assistance programs.
Dealing with Anxiety and Screening Discomfort
Menopause screening can provoke anxiety and discomfort, both physically and emotionally. To address these concerns, healthcare providers should foster a supportive environment, offering clear explanations of what to expect during screenings. Techniques such as mindfulness and deep-breathing exercises can be suggested to help manage anxiety. For physical discomfort, providers can recommend scheduling screenings at times when symptoms are typically less severe and explore the use of local anesthetics or other pain-relief methods when appropriate.
Interpreting Results and Next Steps
Interpreting the results of menopause screenings can be complex. Healthcare providers must ensure that patients understand their results and the implications for their health. Clear communication is crucial, and follow-up appointments should be scheduled to discuss the results in detail. When abnormalities are detected, a prompt and clear plan for further evaluation or treatment should be provided. For normal results, women should be informed about the recommended frequency for future screenings and any lifestyle modifications that may help manage menopausal symptoms.
In conclusion, while menopause screening presents several challenges, thoughtful consideration and proactive management can enhance the screening experience for women. By addressing access barriers, navigating insurance and costs, managing anxiety and discomfort, and ensuring clear interpretation of results, healthcare providers can support women in maintaining their health and well-being during the menopause transition.
Conclusion: Emphasizing the Importance of Menopause Screening
Summarizing the Lifelong Benefits
Menopause screening is a pivotal component of healthcare for aging women. It serves as a proactive measure to identify and mitigate health risks associated with menopause. The benefits of such screenings are multifaceted and extend throughout a woman’s life. Early detection of osteoporosis can lead to timely interventions to strengthen bone density and reduce the risk of fractures. Screening for heart disease allows for the management of cardiovascular health through lifestyle changes and medical treatments. Additionally, identifying menopause-related cancers early, such as breast and ovarian cancer, significantly improves the chances of successful treatment and survival.
Menopause screening also plays a crucial role in the development of personalized treatment plans that address individual symptoms and health concerns. By monitoring overall health and facilitating preventive care, screenings contribute to a better quality of life and can provide mental well-being and peace of mind for women navigating this transition.
Encouraging Proactive Health Management
Proactive health management is essential for maintaining a high quality of life during and after the menopausal transition. Women are encouraged to take an active role in their health by scheduling regular screenings and being vigilant about any changes in their bodies. Understanding individual risk factors, such as family history and lifestyle choices, allows women to make informed decisions about their health care. By doing so, they can address potential issues early on and adopt healthier habits that can prevent or mitigate menopause-related health risks.
Final Thoughts on Partnering with Healthcare Providers
Partnering with healthcare providers is crucial for effective menopause management. Healthcare professionals can offer guidance, support, and access to a range of screening tools that help women navigate this stage of life. Open communication with healthcare providers ensures that women receive the screenings appropriate for their age, health status, and family history. It also allows for the interpretation of results and the discussion of next steps in a supportive and informative environment.
In conclusion, menopause screening is an invaluable tool for safeguarding the health of women as they age. By summarizing the lifelong benefits, encouraging proactive health management, and emphasizing the importance of partnering with healthcare providers, we can ensure that women are well-equipped to manage their health during menopause and beyond.

Bette 100% All-Natural Relaxing Lavender Body Lotion.
Chemical-Free
Your relaxing night time body moisturizer to leave the day’s stress behind. Decompress and wish your body good night with the calming scent of lavender.