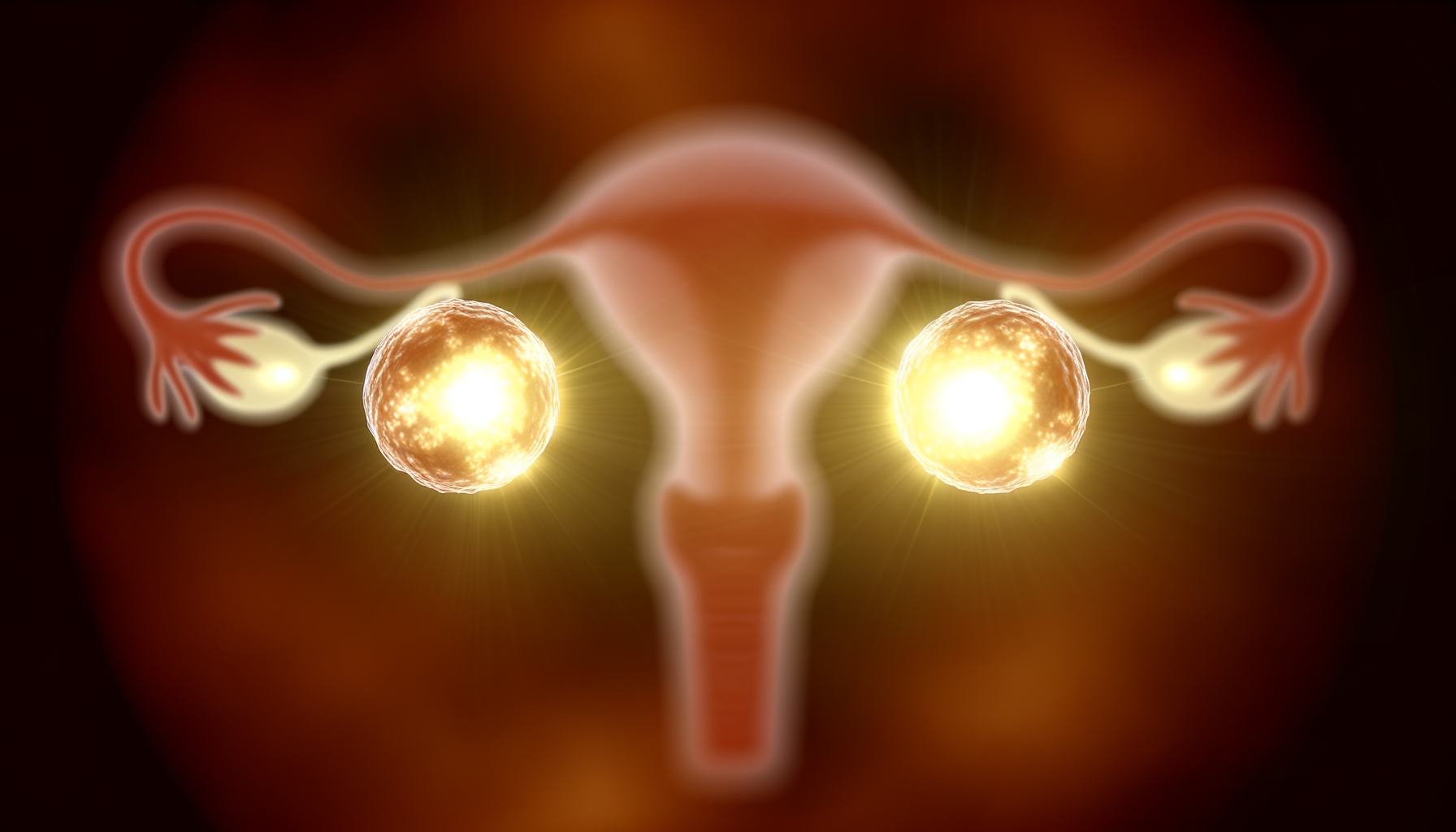
Introduction to Ovaries
The ovaries are a pair of small, almond-shaped organs that play a crucial role in the female reproductive system. Their significance extends beyond reproduction, as they are also endocrine glands that secrete hormones vital to many aspects of a woman’s health. The primary functions of the ovaries include the production of oocytes, or eggs, which are necessary for reproduction, and the secretion of sex hormones, such as estrogen and progesterone, which regulate the menstrual cycle, influence the development of female secondary sexual characteristics, and support pregnancy.
Anatomical Location
Anatomically, the ovaries are situated within the pelvic cavity, flanking the uterus on both sides. They are positioned in the ovarian fossa, a region bounded by the pelvic wall laterally, the ureter and the internal iliac artery posteriorly. Each ovary is attached to the pelvic wall and uterus via the suspensory ligament and the ovarian ligament, respectively. Additionally, the ovaries are connected to the fallopian tubes through the infundibulopelvic ligament, which facilitates the transfer of oocytes from the ovaries to the uterus.
Physical Characteristics
The physical characteristics of the ovaries change throughout a woman’s life, but they typically measure around 3 to 5 cm in length. The outer surface, known as the cortex, is where the development of oocytes occurs, while the inner region, called the medulla, contains blood vessels, lymphatics, and nerves. The surface of the ovary is covered by a layer of epithelial cells called the germinal epithelium, and beneath this lies the tunica albuginea, a dense connective tissue layer. Each ovary contains thousands of follicles, each housing a potential oocyte. These follicles are at various stages of development, and their growth and maturation are tightly regulated by hormonal signals.
Reproductive Functions of Ovaries
Oocyte Production
The primary reproductive function of the ovaries is the production of oocytes, or egg cells, a process known as oogenesis. From the onset of puberty, a woman’s ovaries release one mature oocyte during each menstrual cycle, a process that continues until menopause. This release is the result of a complex interplay of hormones that stimulate the growth and maturation of follicles, each containing a potential oocyte.
Hormonal Regulation
Hormonal regulation is crucial for the proper functioning of the ovaries. The hypothalamus and pituitary gland release gonadotropin-releasing hormone (GnRH), follicle-stimulating hormone (FSH), and luteinizing hormone (LH), which directly influence ovarian activity. FSH is responsible for stimulating follicle growth, while LH triggers ovulation and the formation of the corpus luteum, which secretes progesterone to prepare the uterus for potential pregnancy.
Menstrual Cycle and Ovulation
The menstrual cycle, averaging 28 days, is a series of predictable hormonal events leading to the release of an oocyte. The cycle is divided into two phases: the follicular phase, where FSH promotes the growth of follicles, and the luteal phase, initiated by ovulation and dominated by progesterone production. Ovulation, the release of a mature oocyte from the ovary, typically occurs around day 14 and is a key event in the menstrual cycle, marking the transition between these two phases.
Role in Fertility
The ovaries play an indispensable role in fertility. The release of a mature oocyte during ovulation provides the opportunity for fertilization by a sperm cell. The subsequent hormonal environment created by the ovaries supports implantation and early pregnancy. Without the intricate processes managed by the ovaries, natural conception would not be possible. The health and function of the ovaries are, therefore, central to a woman’s reproductive capability.
Do you know the three main ways that your body gets in touch with harmful chemicals with everyday products? Knowledge is Power!
The Ultimate Detox Guide will tell you how to lower your exposure to harmful chemicals!
Hormonal Output and Effects
Estrogen and Progesterone
The ovaries are not only essential for reproduction but also play a crucial role in the endocrine system, particularly in the production of hormones such as estrogen and progesterone. These hormones are vital for the regulation of the menstrual cycle, the maintenance of pregnancy, and the development of secondary sexual characteristics. Estrogen, primarily estradiol, is synthesized from androgens through the action of aromatase enzymes in the ovarian follicles. It is responsible for the proliferation of the endometrial lining during the follicular phase of the menstrual cycle and works in tandem with progesterone, which is produced after ovulation by the corpus luteum. Progesterone prepares the endometrium for potential implantation and supports early pregnancy. Both hormones exert feedback control on the hypothalamus and pituitary gland, influencing the release of gonadotropins and thereby modulating ovarian function.
Androgens and their Functions
Androgens, including testosterone and androstenedione, are also produced by the ovaries, specifically by the theca cells. While often considered male hormones, androgens play significant roles in female physiology. They serve as precursors for estrogen synthesis and contribute to libido, bone density, and the regulation of follicle maturation. In conditions such as polycystic ovary syndrome (PCOS), androgen levels may be elevated, leading to symptoms like hirsutism, acne, and menstrual irregularities. The balance between androgen and estrogen production is critical for normal ovarian function and overall hormonal homeostasis.
Hormonal Changes During Menstrual Cycle
The menstrual cycle is characterized by dynamic hormonal changes that orchestrate ovulation and menstruation. The cycle begins with the follicular phase, where low levels of estrogen and progesterone from the previous cycle’s end trigger the release of follicle-stimulating hormone (FSH). FSH stimulates follicular growth and estrogen production, which peaks mid-cycle, leading to a surge in luteinizing hormone (LH) and subsequent ovulation. The luteal phase follows, with the corpus luteum forming from the ruptured follicle and secreting progesterone and some estrogen. If fertilization does not occur, the corpus luteum degenerates, hormone levels drop, and menstruation begins, marking the start of a new cycle.

Ovarian Lifecycle
From Birth to Puberty
The journey of the ovaries begins in utero, where primordial germ cells migrate to the developing gonads, multiplying and eventually forming oogonia. By mid-gestation, these oogonia enter meiosis, becoming primary oocytes and investing themselves within primordial follicles. At birth, a female has approximately 1 to 2 million of these follicles, each containing a primary oocyte arrested in the first meiotic division. However, this number declines rapidly, and by the onset of puberty, only about 300,000 to 400,000 follicles remain.
During childhood, the ovaries are relatively quiescent. The primordial follicles exist in a dormant state, with only a small number beginning to grow and develop into primary and secondary follicles. This process, known as folliculogenesis, is independent of gonadotropin stimulation until the approach of puberty. The onset of puberty triggers the hypothalamic-pituitary-gonadal axis, leading to increased levels of follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which are crucial for the next phase of the ovarian lifecycle.
Reproductive Years
With the advent of puberty, the ovaries enter their most active phase. The menstrual cycle commences, driven by the interplay of hormones that regulate the growth and release of eggs and the preparation of the uterine lining for potential pregnancy. Each cycle involves the recruitment of several follicles, although typically only one achieves dominance and proceeds to ovulation. The remaining follicles undergo atresia.
The dominant follicle releases an egg during ovulation, which then has the potential to be fertilized. If fertilization does not occur, the corpus luteum, formed from the remnants of the ovulated follicle, degenerates, leading to menstruation. This cyclical process repeats itself approximately every 28 days and is a hallmark of the reproductive years.
Menopause and its Implications
As a woman approaches her late 40s to early 50s, the number of follicles diminishes, and the ovaries become less responsive to FSH and LH. This transition, known as perimenopause, leads to irregular menstrual cycles and eventually to menopause—the cessation of menstrual periods. Menopause signifies the end of a woman’s reproductive years and is confirmed after twelve consecutive months without a menstrual period.
Menopause is associated with significant hormonal changes, most notably a decrease in estrogen and progesterone production. This can lead to various symptoms, including hot flashes, night sweats, mood swings, and vaginal dryness. Long-term effects of decreased estrogen include an increased risk of osteoporosis and cardiovascular disease. Hormone replacement therapy (HRT) and lifestyle modifications are common approaches to managing menopausal symptoms and reducing associated health risks.
The postmenopausal ovary continues to produce androgens, which can be converted peripherally into estrogens. However, the absence of active follicles and the decline in estrogen levels mark the final stage of the ovarian lifecycle.

THEN IT CONTAINS TOXIC CHEMICALS. WHY RISK IT GETTING SICK? GO CHEMICAL FREE.
Common Ovarian Disorders
Polycystic Ovary Syndrome (PCOS)
Polycystic Ovary Syndrome, commonly known as PCOS, is a hormonal disorder prevalent among women of reproductive age. Characterized by irregular menstrual cycles, excess androgen levels (male hormones), and polycystic ovaries, PCOS affects approximately 1 in 10 women. Women with PCOS may experience symptoms such as acne, hirsutism (excessive hair growth), and obesity. The exact cause of PCOS is unknown, but factors like excess insulin, low-grade inflammation, and genetics may contribute to its development. Treatment options vary depending on whether the patient is seeking to become pregnant and may include lifestyle changes, medications to regulate menstrual cycles, and interventions to manage symptoms.
Premature Ovarian Insufficiency
Premature Ovarian Insufficiency (POI), also known as premature ovarian failure, is a condition where the ovaries cease to function normally before the age of 40. Women with POI may experience menopausal symptoms, including hot flashes, night sweats, and irregular periods. The cause of POI is often idiopathic, but it can be associated with genetic factors or autoimmune disorders. POI can significantly impact fertility, and women with this condition may require hormone replacement therapy (HRT) and other treatments to manage symptoms and address fertility concerns.
Ovarian Cysts and Tumors
Ovarian cysts are fluid-filled sacs that can form on or within the ovaries. The most common types are functional cysts, which are related to the menstrual cycle. These include follicular cysts, which occur when the follicle does not release an egg, and corpus luteum cysts, which form if the follicle does not dissolve after releasing an egg. While most cysts are benign and often resolve on their own, some may cause symptoms like pelvic pain, abnormal bleeding, and pressure on the bladder or bowels. In rare cases, cysts can cause ovarian torsion or rupture, leading to severe pain and potential complications.
Ovarian tumors, on the other hand, can be benign or malignant. Ovarian cancer is a serious condition that is more common in postmenopausal women, but it can occur at any age. Symptoms are often vague and can include abdominal bloating, pelvic pain, and changes in bowel habits. Early detection is crucial for the successful treatment of ovarian cancer, and regular pelvic examinations, along with imaging tests like ultrasounds and blood tests for cancer markers, are important diagnostic tools.
It is essential for women to be aware of these common ovarian disorders and to seek medical advice if they experience symptoms that could indicate an underlying issue. Early diagnosis and appropriate treatment can help manage these conditions effectively and improve overall reproductive health.
Impact of External Factors on Ovarian Health
Chemotherapy and Radiotherapy
The ovaries are highly sensitive to the cytotoxic effects of chemotherapy and radiotherapy, treatments commonly used in cancer management. These therapies can cause direct damage to the DNA of ovarian cells, leading to premature ovarian failure (POF) or diminished ovarian reserve (DOR). The extent of damage is influenced by factors such as the patient’s age, the type and dosage of drugs, and the radiation field and dose. Alkylating agents, for instance, are particularly notorious for their gonadotoxic effects. The loss of ovarian function not only affects fertility but also leads to hormonal imbalances that can have wide-ranging consequences on a woman’s health, including an increased risk of osteoporosis and cardiovascular disease.
Lifestyle and Environmental Factors
Lifestyle choices and environmental exposures play a significant role in ovarian health. Factors such as smoking and exposure to environmental toxins like endocrine-disrupting chemicals (EDCs) have been associated with earlier menopause and reduced ovarian reserve. EDCs, which include compounds like bisphenol A (BPA) and phthalates, can interfere with the body’s hormonal systems, potentially leading to disorders such as polycystic ovary syndrome (PCOS). Additionally, stress and sleep disturbances have been linked to menstrual irregularities and may impact ovarian function through dysregulation of the hypothalamic-pituitary-ovarian (HPO) axis.
Nutrition and Body Weight
Nutrition plays a pivotal role in maintaining ovarian health. Diets rich in antioxidants may help protect ovarian cells from oxidative stress, while those high in processed foods and sugars can contribute to insulin resistance, a common feature in PCOS. Obesity is a well-established risk factor for the development of PCOS and can exacerbate hormonal imbalances and insulin resistance. Conversely, underweight individuals may experience amenorrhea and anovulation due to insufficient energy availability for normal reproductive function. Maintaining a balanced diet and healthy body weight is crucial for optimal ovarian function and fertility.
In summary, the health of the ovaries is influenced by a complex interplay of medical treatments, lifestyle choices, and environmental exposures. Understanding these factors is essential for the prevention and management of ovarian disorders and for safeguarding women’s reproductive and overall health.
By the way, something for you, a little gift!!!
I am just in the middle of publishing my book. It’s about How women can balance their hormones. One part is about food and diet, of course.
Follow this link and enter your email.
I will send you this part of the book for free once the book is published. It has many concrete, practical tips and recipes and will help you feel better during menopause or times of Big hormonal fluctuations.
Annette, Damiva Lead for Health & Wellness

Diagnosis and Treatment of Ovarian Conditions
Diagnostic Techniques
The diagnosis of ovarian conditions often begins with a thorough medical history and physical examination, including a pelvic exam. During this exam, a healthcare provider can check for any abnormalities in the reproductive organs. If further investigation is warranted, blood tests can measure hormone levels to exclude other causes of menstrual irregularities or symptoms mimicking polycystic ovary syndrome (PCOS). Additionally, a transvaginal ultrasound may be performed, using a transducer inserted into the vagina to create images of the ovaries and assess for the presence of cysts or other abnormalities.
Hormone Replacement Therapy (HRT)
HRT is a treatment option for women experiencing symptoms due to decreased hormone production, particularly around menopause. It involves the administration of estrogen and progesterone to alleviate symptoms such as hot flashes, vaginal dryness, and bone density loss. However, HRT is not typically used for the direct treatment of ovarian conditions like PCOS, but rather to manage symptoms associated with hormonal imbalances.
Surgical Interventions
In certain cases, surgical interventions may be necessary to treat ovarian conditions. For example, ovarian cysts that do not resolve on their own or cause significant symptoms may require surgical removal. Laparoscopic surgery is often the preferred method due to its minimally invasive nature. In cases of ovarian tumors, more extensive surgery may be needed. Additionally, ovarian drilling is a procedure sometimes used for women with PCOS who do not respond to fertility medications, where several small holes are made in the ovaries to restore normal ovulation.
Lifestyle Modifications and Support
Lifestyle changes can have a significant impact on the management of ovarian conditions. For women with PCOS, weight loss through a balanced diet and regular exercise can improve the effectiveness of medications and help with infertility. A low-glycemic diet may also help manage insulin levels. Moreover, managing stress and seeking support from counseling or support groups can be beneficial for emotional well-being, which is particularly important given the association between PCOS and increased risk of depression and anxiety.
It is essential for women with ovarian conditions to work closely with their healthcare providers to develop a comprehensive treatment plan tailored to their specific needs. This plan may include a combination of diagnostic techniques, possible HRT, surgical options if necessary, and lifestyle modifications to manage symptoms and improve quality of life.